INTRODUCTION – Tummy Tuck (Abdominoplasty)
Real Results
The tummy tuck (“abdominoplasty”) is one of the most gratifying procedures for the plastic surgeon to do, ranking right up with breast augmentation due to the immediacy of the result and profound effects on patient self-esteem.
A protuberant abdomen is a source of embarrassment. Women typically hide their tummies by leaving their tops hanging out or wearing jackets for camouflage. It does seem unfair that motherhood’s reward should be a stretched-out, unattractive midsection. Similarly, women and men who have lost weight recognize that there is a limit to the contractile ability of abdominal skin. No amount of exercise or dieting can cause this skin to contract.
This procedure is very reliable in meeting patient expectations. Despite the name, “tummy tuck,” which sounds simple and almost trivial, it is a major procedure that produces major results.
Stretch Marks
Stretch marks are an unsolved cosmetic problem, like cellulite. Although lasers have been used to treat stretch marks, the results have been disappointing. This is due to the fact that stretch marks resemble scar tissue on a microscopic level. The normal dermal anatomy is missing. No amount of resurfacing is going to change a scar into skin, which is a very different (and more complex) tissue. The only option is to remove stretch marks surgically and bring skin edge to skin edge. This is somewhat unwelcome news to patients who call the office asking about how to remove stretch marks. They are disappointed that a major (and costly) procedure is the only option.
Fortunately, abdominal stretch marks are often contained on the excess skin flap that is going to be removed with an abdominoplasty. So the same time the skin is tightened, the stretch marks are discarded. Stretch marks below the belly button are eliminated. Any stretch marks on the skin of the upper abdomen, above the level of the belly button, will be moved down to the lower abdomen.
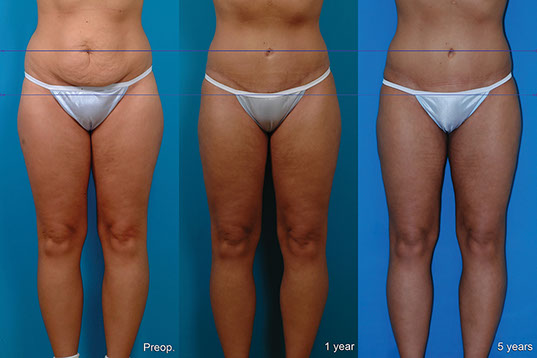
PHOTOS OF FEMALE PATIENTS UNDER 50
B.M., Age 28
Procedure: Abdominoplasty, liposuction of lower body including calves, arms and axillae, breast lift and implants.
Before, 1 year, 5 years after
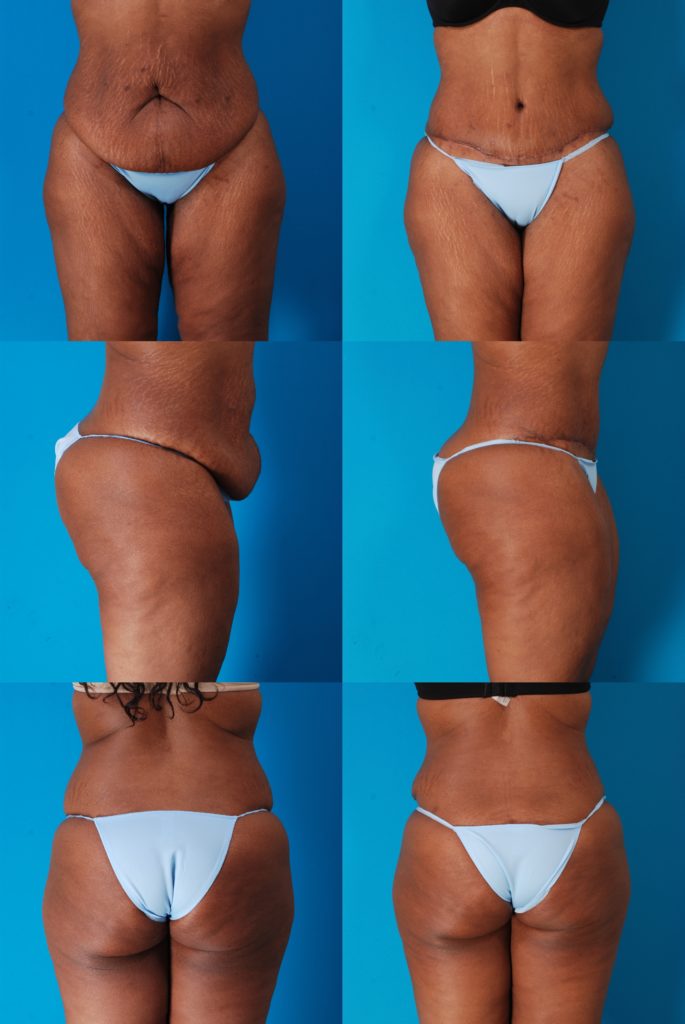
S.M., Age 29
Procedure: Abdominoplasty, liposuction of abdomen, flanks, and outer thighs, and buttock fat injection.
Before, 3 months after, 3½ years after
A.J., Age 30
Procedure: Abdominoplasty, liposuction of abdomen and flanks. This patient had mesh inserted at a previous operation elsewhere.
Before, 6 weeks after
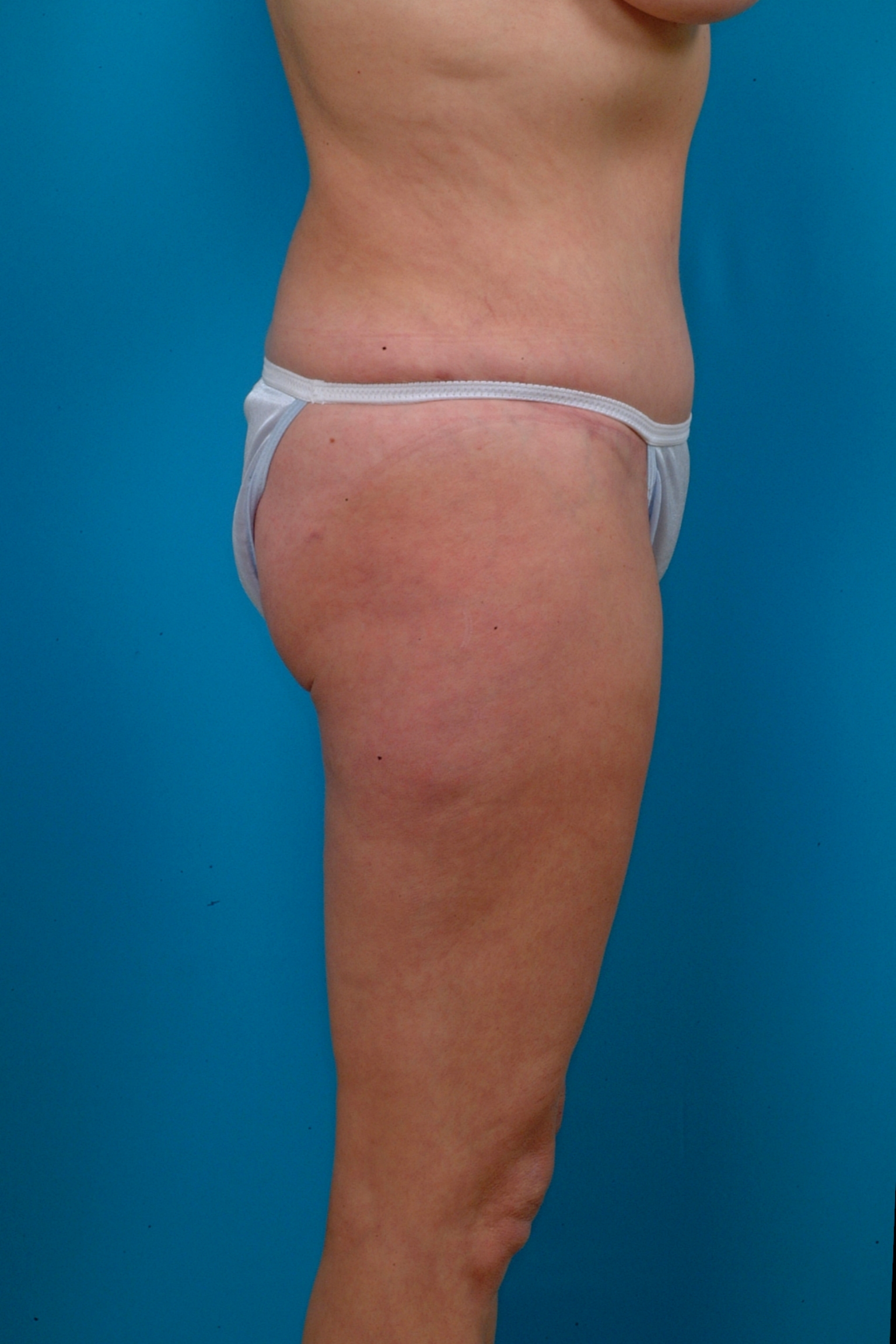
S.R., Age 32
Procedure: Abdominoplasty, liposuction of lower body.
Before, 4½ months after.
N.T. Age 32
Procedure: Abdominoplasty, liposuction of lower body, arms and axillae, and breast augmentation, 6 Months
A.C., Age 33
Procedure: Abdominoplasty, liposuction of abdomen and flanks
8 months
A.H., Age 34
Procedure: Abdominoplasty, liposuction of abdomen and flanks.
Before, 3 years after
A.T., Age 34
Procedure: Abdominoplasty, liposuction of abdomen and flanks. This patient had a major abdominal deformity after having 4 children.
Before, 3 months after
R.S., Age 39
Procedure: Abdominoplasty, liposuction of abdomen, breast lift and implants.
Before, 10 months after
J.C., Age 39
Procedure: Abdominoplasty, augmentation/mastopexies, liposuction of abdomen, flanks, arms and axillae. Additional liposuction and buttock fat injection at a separate time.
Before, 6.5 years after
M.G., Age 40
Procedure: Abdominoplasty, liposuction of abdomen, flanks, arms and axillae
1 year
S.A., Age 41
Procedure: Abdominoplasty, liposuction of abdomen, flanks, and inner thighs
Before, 3 months after
S.S., Age 44
Procedure: Abdominoplasty, liposuction of abdomen, flanks, inner thighs, and axillae, breast reduction, buttock fat injection.
Before, 2 months after
R.K., Age 44
Procedure: Abdominoplasty, liposuction of abdomen, flanks, inner thighs, arms, and axillae.
Before, 6 months after
Mommy Makeover
S.H., Age 46
Procedure: Abdominoplasty, liposuction of lower body, arms and axillae, breast lift and implants, and buttock fat injection.
Before, 1 year after
K.M., Age 48
Procedure: Abdominoplasty, liposuction of abdomen and flanks.
Before, 8 months after
S.N. Age 49
Procedure: Abdominoplasty, liposuction of abdomen and flanks. 3 Months
S.N. Age: 50
1 Year After
PHOTOS OF FEMALE PATIENTS OVER 50
T.W., Age 52
Procedure: Abdominoplasty, secondary liposuction of abdomen, flanks, arms, and axillae, and touch up buttock fat injection.
This patient underwent liposuction and buttock fat injection followed 15 months later by an abdominoplasty and secondary liposuction.
Before, 3 months after
F.W., Age 55
Procedure: Breast reduction, abdominoplasty, and liposuction of abdomen, flanks and inner thighs, and buttock fat injection.
Before, 3 months after
K.M., Age 56
Procedure: Abdominoplasty, liposuction of lower body, arms, and axillae, and buttock fat injection.
Before, 3 months after
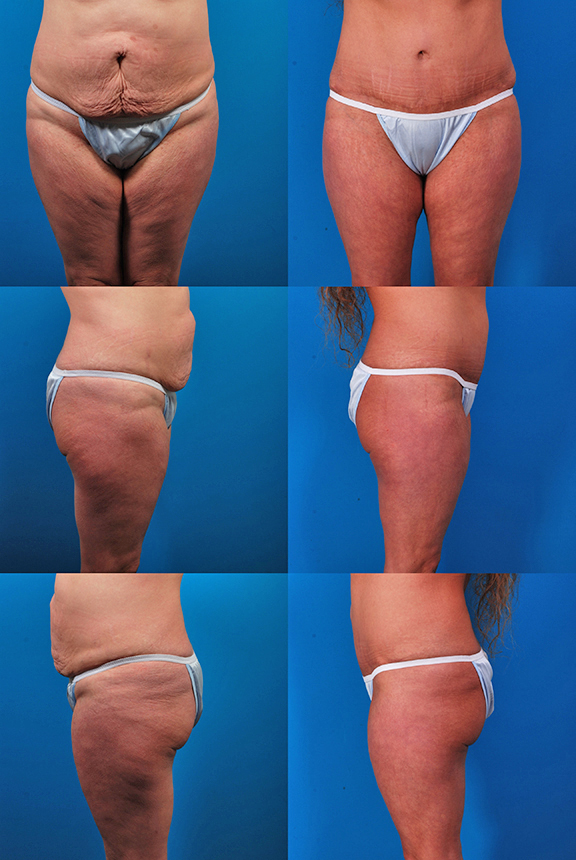
L.P., Age 58
Procedure: Abdominoplasty, liposuction of lower body, arms, and axillae, submental lipectomy.

Before, 6 months after
J.G., Age 63
Procedure: Abdominoplasty, liposuction of lower body.
Before, 3 months after
PHOTOS OF MALE PATIENTS
C.M., Age 20
Procedure: Abdominoplasty, liposuction of abdomen, flanks, inner thighs, and axillae. Touch-up 2 years later: flanks.


Before, 2½ years after (3 months after touch-up)
K.K., Age 37
Procedure: Abdominoplasty, plus outer thigh and buttock lift (Lower body lift). Liposuction of abdomen, flanks, and breasts.

Before, 5 months after
W.A., Age 49
Procedure: Abdominoplasty and touch-up liposuction of flanks and abdomen.
Before, 5 months after
How It Is Done
Abdominoplasty and Anesthesia
Traditionally, abdominoplasties have been performed under general anesthesia, including paralysis, intubation, and ventilation—the maximum degree of anesthesia. However, this operation may be performed under unconscious sedation, using an LMA and propofol (Diprivan) infusion, just like other cosmetic procedures. This modified type of anesthetic avoids possible problems sometimes caused by traditional general anesthetics.
After the patient is asleep, the abdomen is infused with a dilute solution containing bupivacaine, a long-acting local anesthetic, and epinephrine to reduce blood loss. By injecting the abdomen this way and then allowing time for the epinephrine to constrict the small blood vessels, there is a remarkable reduction in bleeding at surgery. Patient comfort is enhanced with the use of bupivacaine, which continues to work for many hours after surgery. This local anesthetic also reduces the amount of anesthetic necessary during surgery, so that the patient recovers faster afterward.
Surgery Center
While abdominoplasties have been traditionally done in a hospital setting with an overnight stay, they are being done more commonly today in ambulatory surgery centers. This is made possible by advances in technique and anesthesia to reduce surgery times, restrict blood loss, improve pain management, and shorten recovery times. We recognize the importance of early ambulation to help avoid blood clots. Also, treatment in outpatient surgical settings helps contain costs and make it more affordable.
The Incision
The incision for a tummy tuck is long, running from hip to hip. Patients are concerned about it before surgery but don’t seem to mind after surgery. The incision needs to be long enough to allow removal of a wide apron of excess skin. The shorter the incision, the less skin may be removed. Patients readily agree that it is better to make the incision a little longer and remove extra skin, than leave unsightly puckering at each end. It is important for the incision to be low. A common surgical error is to place the incision too high, so that it is above the bikini line. Some patients who have had previous abdominoplasties complain about a high-riding scar that is hard to hide. It may be possible to lower the scar at a subsequent procedure, but obviously this is best avoided.
Why Don’t All Plastic Surgeons Place the Incision Low, Within the Bikini Line?
A low incision is not usually a problem in a patient with a large apron of extra skin. It is more difficult in the thin patient with less loose skin. Of course, this is usually a discriminating patient that is going to want a low incision that she can hide. The difficulty in placing the incision low is that the upper margin of the skin to be removed is fixed at the level of the belly button (if a vertical scar is to be avoided). The lower the incision is placed, the more skin is removed between this incision and the level of the belly button. The wider this distance is, the more the upper skin flap needs to come down to meet it. Moving this upper flap down to meet the lower skin edge can be difficult unless the operating table can be adjusted to provide flexion at the hips by bending in the middle. Also, the tighter the repair, the more the patient will be stooped over after surgery. Deep fixation sutures are used to prevent the pubic tissue from being dragged up, bringing pubic hair up onto the abdomen (not good). Experienced plastic surgeons use these technical maneuvers to keep the incision low, avoid upward traction on the hair-bearing pubic skin, and avoid a vertical scar, delivering the best possible cosmetic result.
A Vertical “Inverted-T” Scar Is to Be Avoided, Because It Is Unattractive.
One of the benefits of an abdominoplasty is the capability of removing unsightly old scars, particularly vertical scars that may leave an unsightly cleavage, giving the abdomen the unwelcome appearance of buttocks. These old scars are contained in the extra skin that is discarded.
Abdominoplasty incisions have been made in the shape of a W (I used to do this.), in the shape of bicycle handlebars, or as a gentle concave curve like a saucer. The gentle curve is the most attractive scar, if a scar can be attractive.
Most surgeons mark the incision with the patient standing before surgery. The “photo panties” are used as reference along with the natural skin creases (the “inguinal crease”). The incision courses below any existing scars from previous C-sections or other surgery. This way, any existing lower abdominal scar is removed along with the extra skin. Typically, the new scar ends up at about the same level as an old C-section scar, because it is pulled up a little by tension from above. For patients with an existing C-section scar, the trade-off in scarring is limited to the extra length of the abdominoplasty scar beyond what they had already from the C-section scar and the umbilical scar around the belly button.
One of the benefits of an abdominoplasty is the capability of removing unsightly old scars, particularly vertical scars that may leave an unsightly cleavage, giving the abdomen the unwelcome appearance of buttocks. These old scars are contained in the extra skin that is discarded.
A horizontal elliptical excision is performed, removing the skin and fat from the lower abdomen. All the skin from the level of the belly button (“umbilicus”) to the pubic area is removed. The skin flap is released from the underlying muscle all the way up to the lower border of the rib cage (“costal margin”) to allow the remaining skin of the upper abdomen to be pulled like a bed sheet down to the lower incision, which is tucked just inside the bikini line. This is how a vertical scar is avoided. It is necessary to flex the hips to do this (the operating table is adjusted to flex the hips). The lower the incision line, the more the hips must be flexed to allow this flap to reach.
It is also important for the surgeon to anchor the flap with deep sutures. This helps to prevent upward pulling on the pubic skin which can displace pubic hair upward, which is obviously undesirable. The deep fascial closure also helps preserve a flat skin contour, and avoid a depression along the incision, which can create a ledge just above the incision line. It also helps take some of the tension off the skin closure, optimizing the scar.
Mini-Abdominoplasty
Patients often ask about a mini-tummy tuck. They know that there is a long scar with a regular tummy tuck and wonder if a “mini tummy tuck” might offer the best combination of results and minimal scarring.
How is a mini-tummy tuck different from a regular tummy tuck? In a regular tummy tuck, or “full abdominoplasty,” the umbilicus is released from the surrounding abdominal skin and then reintroduced through a new hole once the skin drape has been pulled down. In a mini-tummy tuck, the umbilicus is not released. It stays attached to the surrounding abdominal skin and can be pulled down due to skin tension from below. A much smaller ellipse of skin is removed from the lower abdomen. The scar is shorter and ends up looking much like a C-section scar. There is no tightening of skin of the upper abdomen because the umbilicus remains anchored, preventing any tightening of the skin above it. It may be possible to tighten the muscles of the lower abdomen but it is difficult to tighten the muscles above the level of the umbilicus because the upper abdomen is not exposed.
So a mini-tummy tuck is really just a removal of extra lower abdominal skin. It does not treat the upper abdomen. If the patient is concerned about loose skin above the belly button, or a roll that borders the belly button, and most are, she will not be adequately treated with a mini-tummy tuck. Not surprisingly, I perform very few mini-abdominoplasties, about one for every 100 full tummy tucks.
Muscle Repair
One of the most satisfying components of an abdominoplasty is the muscle repair. Pregnancy and weight gain stretch the abdominal wall. The two rectus abdominis muscles, which are oriented vertically in the abdomen, are stretched apart.
The muscles become bowed apart, often separated by several inches at the level of the umbilicus. Exercise cannot bring these muscles back together. They can only be realigned surgically. This is done by sewing the muscle borders together, up and down the abdomen like a zipper. Actually, the “fascial” envelope that contains the muscle is sewn together, not the muscle itself because muscles are too elastic and don’t hold sutures well. After surgery, and after the swelling has gone down, the borders of the muscle can now be seen, moved in closer to the midline. The muscles have been replaced in their original position, where they were prior to being stretched apart from pregnancy or weight gain. It is an anatomical restoration. This realignment also improves the mechanical advantage of the abdominal muscles. This can help alleviate back pain due to muscle imbalance. It is possible that this may also help bowel function in some patients. The muscle repair helps flatten the abdomen and correct excessive protuberance. It is important to recognize that the abdomen is not typically flat, even in lean, muscular individuals. However, the muscle repair can correct excess protuberance and leave a pleasing gentle convexity.
What To Expect After Surgery
Other questions:
Back Pain:
Better 33%
The Same 66%
Worse 1%
Bowel Function:
Better 21%
The Same 73%
Worse 6%
Comparisons:
Abdominoplasty compared to a C-section (19 pts.):
Pain:
Better 21%
The Same 32%
Worse 47%
Recovery:
Better 16%
The Same 26%
Worse 58%
Abdominoplasty compared to a hysterectomy (10 pts.):
Pain:
Better 40%
The Same 20%
Worse 40%
Recovery:
Better 30%
The Same 20%
Worse 50%
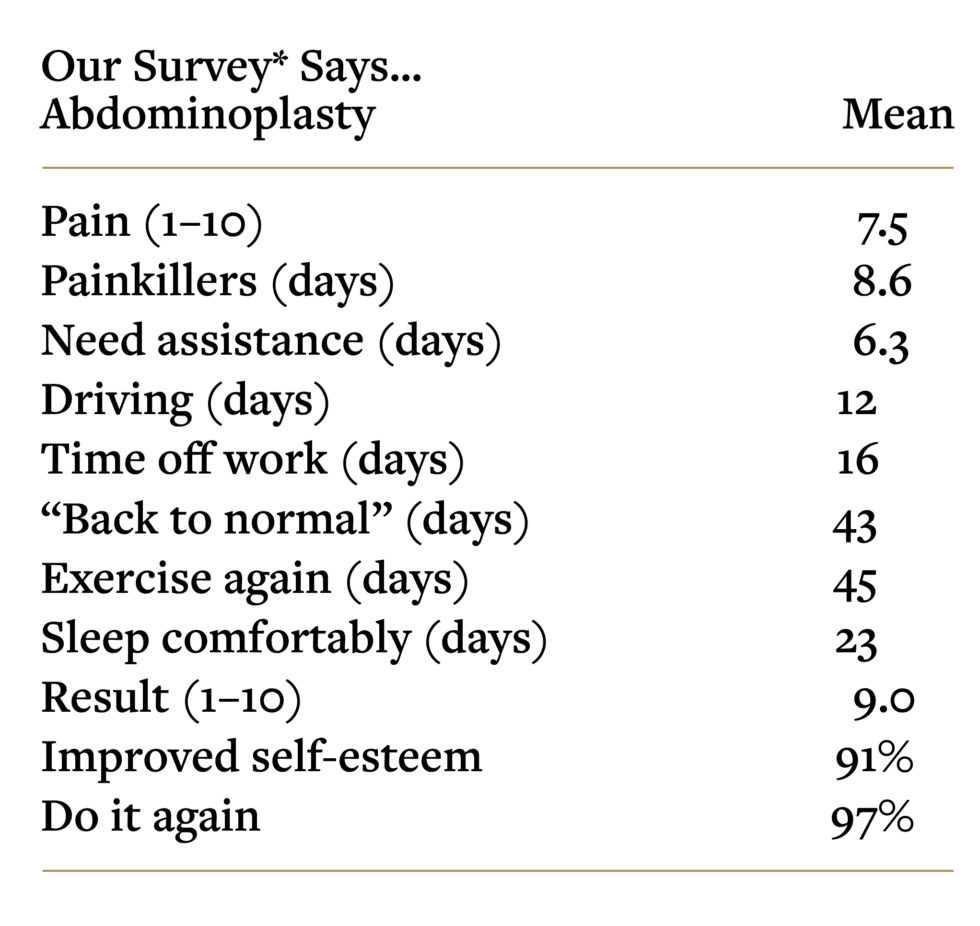
*Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129:965–978; discussion 979–980.
Recovery
Patients in the recovery room after surgery are often already gratified by the change in their abdominal contour. Like breast augmentation, this immediate gratification helps to offset some of the discomfort. The local anesthetic is still working, and will continue to work for several hours.
The nurse will help you get up and walk. You are in a “stooped” position. This is made necessary by the tightness of the abdominal skin repair. The nurse will help you to the bathroom. It is not unusual to use a catheter in the recovery room if patients are unable to void. The nurse will help you put on your clothes. Your caretaker will be given instructions. This includes taking care of the drain. Most patients are in the recovery room for about an hour.
The Drain
I use only one drain. The drain will accumulate bloody fluid after surgery. It is important to know that this fluid is mainly tissue fluid with a small amount of blood. It is quite diluted, so don’t worry that you are losing a lot of blood from the drain. You empty the drain when it is about a third or half full. If it gets too full, it will lose suction. It should always be collapsed, which indicates it is working to produce suction.
Keeping the Hips Flexed
You will need to keep your hips flexed to avoid too much tension on the wound closure. You will do this automatically. I tell husbands (and occasionally a wife for a male patient) to help support your legs when you swivel into the car because it is hard for you to lift your legs up.
At home, a recliner works well because it provides elevation of the upper body and flexion of the hips. You can also use a bed, but you will need to put several of pillows under your back, shoulders and head, and also one under your knees to maintain a flexed position at the hips. Some patients purchase a foam wedge and use it for their upper body. You will need some help at first getting in and out of bed and up to go to the bathroom.
Up Walking Right Away
Patients typically urinate several times during the night after surgery. This is normal. You received fluids in surgery both through the I.V. line and by injection into the tissues. The kidneys work to remove this fluid during the first 24 hours or so after surgery. These short trips up to the bathroom are helpful because they make you use your legs. This ambulation helps to avoid prolonged immobilization, reducing the risk of blood clots after surgery.
Follow-Up
Usually, I see patients the day after surgery. This helps to ensure that they are mobile and getting up and around. The dressing is removed at this visit. The nurse takes the garment down part way to do this and then places gauze along the incision line. Also, a layer of gauze is placed under the drain, between the drain and the skin. This is done to avoid pressure from the drain on the skin. If this isn’t done, the drain might leave a dent or even a scar on the skin. You should start bathing the day after surgery, or at the latest, the second day after surgery. You can get into a bathtub or use a shower. You will need some help the first couple of times. While you are bathing, wash the garment. The Band-Aids can come off the day after surgery, or earlier if any are saturated. Leave the semi-transparent white tapes (“Steri-Strips”) along the incision lines. These will come off after about a week. The smaller ones at liposuction sites can come off in a few days.
I see patients 3 or 4 days after surgery to remove the drain. They imagine that this must be painful. In fact, it only takes a few seconds to pull out the drain, and usually this is not particularly painful, less uncomfortable than removal of the dressing the day after surgery. The drain site heals on its own in a few days. All you need to do is use a gauze dressing at the site to absorb any fluid that continues to drain.
Sutures
The abdominoplasty sutures dissolve on their own. The belly button sutures usually come out 2 weeks after surgery. The skin is still numb so this does not hurt.
Discomfort and Numbness
Patients often report discomfort in their lower back. This may be due to liposuction used to treat the flank areas, and possibly the stooped posture after surgery. The tummy feels uncomfortably tight. The skin of the lower abdomen is numb, because sensory nerve branches have been traumatized or divided in performing the tummy tuck. It takes months for the feeling to gradually come back and it is possible to have some persistent numbness, although this is not distressing to patients, who are very gratified by the appearance of their tummy.
Umbilical Appearance
No doubt it would be possible to devote an entire book to umbilical aesthetics. The appearance of the umbilicus today is taking on greater importance, as the midriff is now more exposed. A small, oval umbilicus with a fold over the top part is ideal. It is important for the surgeon to avoid having the umbilicus point upward after surgery. If anything, it should be oriented slightly down. A large, wide umbilicus is undesirable. Ideally, the scar is concealed in a natural fold or tucked in the inside, although this is not always possible, especially in very lean patients. It is possible to make the opening too small, which makes it difficult to clean the belly button. This problem can be treated with a release under local anesthetic if it occurs.
It is not unusual for the umbilical scar to widen, especially on the sides. If this happens, the umbilicus may be revised as an office procedure under local anesthetic. The wider scar tissue is simply excised. This is done at least several months after surgery, when the wound tension has been relieved. With less tension on the scar, there is less likelihood of recurrence. However, for some unfortunate patients, scar hypertrophy or even keloids can be a recurrent problem.
Abdominoplasty Scar
The downside of a full abdominoplasty is the long incision. However, the extra inches at the lateral ends usually heal the best because this portion of the incision has the least tension, and the incision may be kept within the bikini line, hidden in the natural inguinal crease. It turns out that this longer scar is not usually objectionable. A full abdominoplasty requires a scar that goes around the umbilicus. This is necessary because a large flap of skin is mobilized and needs to be freed of its attachment at the umbilicus. There are some patients who form hypertrophic scars and this can be a bothersome complication. Fortunately, the rewards in improved body contour are almost always a worthwhile trade-off even when scarring is more noticeable. With time, scars tend to improve. They are raised and reddened at first, but gradually soften, flatten, and fade. This can take over a year.
“Dog Ears”
This term refers to puckering at the end of any surgical incision. Dog ears do sometimes occur after abdominoplasty. Whenever a surgeon removes extra skin, usually with an elliptical incision, there is a pucker at the end of the incision that develops when the skin edges are approximated, due to tissue bunching beyond the end of the incision. This is a geometric reality. These puckers may be avoided by making the incision longer and more tapered. The more tapered the end of the incision, the less redundancy there will be when the edges are brought together. However, this is at the expense of a much longer scar. It turns out that puckering of human skin tends to improve with time. Unlike cloth fabric, human skin is a dynamic tissue capable of contraction. Small puckers usually flatten out with time. The surgeon’s job is to make the incision long enough to avoid a dog ear, but also keep it as short as possible. This judgment comes from experience. It is always possible to come back and remove an extra little pucker in the skin if necessary, under local anesthetic in the office. Sometimes extra fat persists in this area, and may be treated with a touch-up liposuction, or simply excised with the extra skin. There is minimal downtime after this touch-up procedure.
Complications
Infection
Although infection is very unusual after liposuction, it happens from time to time after abdominoplasty. It presents with increasing redness (“cellulitis”), fever, and possibly a purulent drainage from the incision. A yellow drainage is normal and to be expected, but a greenish or white drainage or any foul-smelling drainage is not. This indicates infection. Antibiotics are prescribed and any purulent drainage is cultured. Infections typically respond to antibiotics, although drug-resistant strains of Staphylococcus (MRSA) are becoming more prevalent. It may be necessary to drain an abscess and irrigate the wound, which is done under local anesthesia in the office.
Seroma
A fluid collection under the skin is called a seroma. If the swelling seems to be getting worse, this may indicate that such a fluid collection has developed. Patients may reasonably wonder why the drain did not prevent such a problem. Should the drain simply be left in longer? The problem is that the longer the drain is left in, the greater the risk of infection. That is why we prefer to remove the drain 3 or 4 days after surgery. If a seroma develops, it is treated by injecting a needle into the swollen area and draining off the fluid. This maneuver immediately corrects the excess swelling and patients are more comfortable. Fortunately, it is not particularly painful because the skin where the needle is introduced is still numb. This aspiration typically needs to be repeated several times. Eventually, the lymphatics start working again to absorb the fluid and it is no longer necessary.
Surgeons find this problem a nuisance (as do their patients) and try to avoid it by preserving the “areolar” tissue layer over the abdominal wall during the abdominoplasty. The skin undermining is limited to just what is necessary to gain adequate release of the flap. (This also helps preserve blood supply and sensation). I personally find it helpful to avoid the use of cautery during the dissection. Pretreatment with the Marcaine/epinephrine solution reduces blood loss sufficiently to allow dissection using a scalpel (as well as providing long-lasting anesthesia of the tissues). This technique limits tissue injury and inflammation that might otherwise cause more fluid release. The risk of seroma is minimized. In my series of patients the seroma rate was a very manageable 5.4% (Swanson E. Prospective clinical study of 551 cases of liposuction and abdominoplasty performed individually and in combination. Plast Reconstr Surg Glob Open 2013;1:e32). This rate compares with much higher rates in other series—as high as 60%.
Draining a seroma in the office after an abdominoplasty.
Hematoma
Hematomas (collections of blood) can occur after an abdominoplasty, and can possibly necessitate a return to the operating room for evacuation, although this is very unusual. Prompt recognition and treatment is the key. Surgeons who routinely prescribe blood thinners report increased bleeding and hematomas. I prefer safer methods to reduce the risk of blood clots (Swanson E. The case against chemoprophylaxis for venous thromboembolism prevention and the rationale for SAFE anesthesia. Plast Reconstr Surg Glob Open 2014;2:e160).
Deep Venous Thrombosis (DVT)
A blood clot in the deep vein of the thigh (“deep venous thrombosis”) is a serious and potentially life-threatening complication of surgery. The risk of a DVT is that a clot may break off, travel to the lungs and cause a pulmonary embolus, which can be fatal. The risk is increased by immobilization of the lower extremities. It can even occur in patients after long plane flights. The risk may be reduced with the avoidance of paralysis (so as to preserve the calf muscle pump) and early ambulation. My patients are turned from side to side during surgery (during the liposuction treatment) to keep the legs mobile. The prone position, which exerts pressure at the hips, is avoided entirely.
Some surgeons advocate the use of blood thinners (Lovenox. Xarelto, or Eliquis) immediately after surgery, but their use has to be balanced against the risks of easier bleeding after surgery. I believe the risks outweigh any possible benefits.
Ultrasound Surveillance
Doppler ultrasound screening examinations provide a highly accurate method to detect early blood clots and treat them before they become dangerous. It avoids routine anticoagulation in patients who do not need it. I use it on all abdominoplasty patients
- Swanson E. Ultrasound screening for deep venous thrombosis detection: Prospective evaluation of 200 plastic surgery outpatients. Plast Reconstr Surg Glob Open 2015;3:e332.
- Swanson E. Ultrasound surveillance offers a safe and effective method for venous thromboembolism prevention in plastic surgery patients. Aesthetic Plast Surg. 2020;231:783–784.
- Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96.
This 39-year-old woman is seen before surgery, 2 weeks after an abdominoplasty and liposuction of her lower body, and 3½ months after surgery. She developed swelling of the left lower extremity 9 days after surgery. A Doppler ultrasound scan revealed a deep venous thrombosis. She did not develop pulmonary emboli. She was treated with anticoagulation and made a full recovery.
Skin Loss
This 63-year-old nonsmoker had a tummy tuck and liposuction. She had an old scar across her right upper abdomen, from removal of her gall bladder 35 years ago. Prior to surgery, we discussed the fact that this scar would compromise circulation to the abdominal skin and possibly cause some skin loss, which is exactly what happened. The wound healed in gradually on its own. The patient was pleased despite the scar (which could have been revised but the patient did not find it a problem). The key to her satisfaction was knowing that this complication could occur and accepting that possibility.
Smoking
Abdominoplasty and ultrasonic liposuction of lower body.
Excessive Scarring
The central portion of the abdominoplasty may spread, depending on the patient’s healing characteristics and wound tension. Any factor that interferes with wound healing, such as an infection or skin loss (see above) can contribute to a wider, more conspicuous scar. After 6 months to a year, the tension has been relieved. At this point, the scar may be revised.
Revision of previous abdominoplasty and liposuction of abdomen, flanks, and inner thighs.
This patient had an unsightly scar from a previous tummy tuck performed elsewhere. The scar ran slightly above her bikini line and had widened. There was a contour depression associated with it. At surgery, I revised the scar, using anchoring sutures to keep it low and avoid upward migration. A deep tissue repair corrected the contour deformity. Liposuction was used to correct her muffin top deformity of the flanks and also taper the inner thighs. The umbilicus was lowered slightly, correcting its unnatural orientation.
Care After Surgery
- Avoid straightening your hips fully. Walk in a stooped position to reduce tension on the abdomen.
- You can take stairs, but with assistance.
- At night, be sure to keep your hips flexed and sleep on your back (“supine”), not on your side. A recliner works. Otherwise, use several pillows under your upper body and tuck one under your knees.
- The suction drain needs to be emptied when it is about one-third to one-half full. After emptying, be sure to squeeze the bulb when closing the valve. The bulb should stay collapsed. This indicates that it is creating the suction needed to draw fluid off the abdomen. Don’t be surprised if you have to empty it several times the night after surgery. This is normal. Although it looks like a lot of blood is coming out, it is mainly fluid (not much blood is needed to turn the fluid red). The drainage typically slows down after the first 24 hours.
- You should be getting up to urinate every 3 hours or so. Be sure to drink adequately to stay well hydrated. These trips to the bathroom are also helpful to get you up and moving. This helps prevent blood clots from developing in your legs.
- Your tummy will feel very tight. This is normal.
- Sometimes there is some blood-tinged drainage around the drain tube. Simply tuck some gauze in to absorb it and confirm that the suction drain is working. Be sure there are no kinks in the tubing and the bulb is collapsed.
- You can unzip the garment (if you are wearing a girdle) partly at the top if it is digging in to your sides. If the garment is uncomfortably tight in the inner thighs, you can cut the margin to relieve any uncomfortable constriction. Similarly, if the garment is too tight at the knees, it can be cut to release any tourniquet effect, although this is rarely necessary.
- Some bloody drainage into the dressing and through to the garment is normal after surgery. However, if this increases, or if the dressing becomes saturated, notify the office.
- You will be seen the day after surgery in the office. The dressing will be removed. When you go home you can bathe later that day, or at the latest, the next day. It is okay for the tummy to get wet. Just put the drain over the edge of the bathtub or hold it in the shower.
- Be careful when you take off the garment. You may feel light-headed at first. It is best to take off the garment and then sit for several minutes before standing. This allows your body time to adjust to the new position. If you feel faint when standing, immediately lie down, even if this means lying down on the bathroom floor. Much better to lie down than fall down. The lightheadedness will go away. Don’t try to fight the faint feeling. Give in and lie down. This is typically important the first few days after surgery. Later on, this is usually not a problem.
- Keep a layer of gauze between the drain tube and the skin when you have the garment on. This will avoid an indentation which could possibly leave a mark.
- Sometimes the tightness of the abdomen can cause heartburn. An antacid can help.
- Don’t be surprised by swelling above the level of the garment. It is not possible to provide compression over the upper abdomen, because this might restrict breathing. Don’t worry, this swelling will go down and you will not be left with a ledge over the top of the garment.
- Bruising usually occurs in the flanks and back due to the effects of gravity.
- Usually the discomfort is in the flanks and back and caused by liposuction, which is usually performed simultaneously with the abdominoplasty.
- Wash the garment and then dry in a no-heat dryer. Keep the bottom of the garment, at the knees, partially zipped up so the garment does not get completely tangled up in the wash.
- Avoid any activities that stress the abdominal muscles.
- Avoid taking too many painkillers. A side effect is nausea. It is very uncomfortable to vomit after a tummy tuck. So don’t take more than two tablets every 4 hours. You can take one and a half painkillers or substitute a Tylenol (acetaminophen) for the second painkiller. It is important to treat pain, but avoid overtreatment, which can produce nausea. Ibuprofen or acetaminophen may be used as an alternative to the prescription painkillers if the pain is not too severe. Non-steroidal anti-inflammatories avoid the side effects of narcotic painkillers, such as constipation, nausea, and sedation. Be sure not to exceed the maximum recommended dose (4000 mg/day for acetaminophen or 3200 mg/day for ibuprofen).
- It is important to avoid nausea because vomiting after an abdominoplasty is painful and can disrupt the sutures that are holding the muscles together. Zofran (ondansetron) is prescribed to prevent and treat nausea, but the most important factor is narcotic usage, so try to use just what you need and no more. The Zofran tablet dissolves under your tongue. You can take one every 6 hours as needed.
- If you do feel that you are going to vomit, hold your tummy with a pillow to support the muscle repair. You might feel a stitch pop. Don’t worry, this is not dangerous, and I use extra sutures to repair the muscles for this reason.
- Most of the sutures dissolve. The belly button sutures are typically removed about 2 weeks after surgery. The Steri-Strips along the abdominoplasty incision are left on for about a week, but don’t worry if some of them come off sooner. You can take the Band-Aids off the liposuction incisions when you first bathe after surgery (or sooner if any are saturated). Usually, you don’t need to replace these, but if there is any drainage go ahead and put on another Band-Aid.
- There will be swelling above the garment, where there is no compression, and along the lower abdomen. This swelling along the incision line can feel very firm. Gradually it softens. It takes a few months for this swelling to go down and for the tissues to feel soft again.
- The pubic area will be swollen and may be bruised. This is from liposuction (if this area is treated) or just from fluid and blood settling after the abdominoplasty. Even the labia (or scrotal area in men) can be swollen and bruised. Don’t be alarmed by this.
FAQs
Q: What can I do about my stretch marks?
A: Nonsurgical treatment is ineffective. Stretch marks on the lower abdomen can be eliminated with a tummy tuck. Stretch marks on the upper abdomen are moved down to the lower abdomen.
Q: Should I wait until I am done having children before having surgery?
A: It makes sense to wait until you are finished having children so that you don’t stretch the skin again and possibly stretch out the muscle repair too. For women who are unsure about future pregnancies, a judgment call needs to be made—the advantages of having the results now, against the possibility of having to do another tightening procedure later on. Of course, limiting weight gain with pregnancy will help. The abdominoplasty itself does not affect your ability to get pregnant or cause any problem with expansion of tissues during pregnancy. Many of my patients have gone on later to have pregnancies, but very few seem to return for revision of their tummy tucks.
Q: I’ve had previous abdominal surgery. What are the risks?
A: The abdominoplasty does not involve opening the abdominal cavity that contains the organs. Sometimes patients are concerned about adhesions— internal bands of scar tissue that can develop around organs and cause problems. Because the peritoneum is not entered, there is no risk of adhesions from an abdominoplasty.
Q: Do you use a pain pump?
A: Of course, this is not a “pain pump” (patients are having enough of that already) but a “local anesthetic pump” that delivers small amounts of local anesthetic into the surgical wound after surgery using a catheter and a pump. A pain pump sounds like a reasonable and humane measure to improve patient comfort. However, a study showed similar pain scores and use of prescription painkillers in patients with and without these pumps after abdominoplasty, so they don’t appear to be sufficiently beneficial to justify the added nuisance of looking after it, the expense, and occasional complications. Possible reasons for its ineffectiveness are a lack of penetration of the muscle fascia, and a compromised distribution in the wound due to gravity and suction drains used after surgery that may drain off the local anesthetic solution. I prefer to infuse the tissues with a long-lasting local anesthetic solution that penetrates the muscle and is slowly released by fat cells into the tissues. I call this a “physiological pain pump” (Swanson E. A physiological pain pump for abdominoplasty: An alternative to regional blocks and liposomal bupivacaine. Plast Reconstr Surg. 2015;136:714e–716e).
Q: Do you use that new long-lasting local anesthetic?
A: Liposomal bupivacaine (Exparel) is being used by some plastic surgeons. However, its diffusion into the tissues is limited. I prefer using bupivacaine in a “superwet” solution that permeates the tissues and is slowly released by the patient’s own fat cells (as described above).
Q: I have a belly button hernia. Can it be repaired simultaneously?
A: This can be repaired at the same time as the abdominoplasty. Also, excessively wide belly buttons can often be tightened into more attractive, smaller “innies.”
Q: Do you do many tummy tucks on men?
A: Not as many as women, of course, because of the effects of pregnancy. However, any patient, male or female, who has lost weight, or who otherwise has poor skin tone of the abdomen, can benefit.
Q: How much weight will I lose?
A: The weight of the abdominal tissue that is removed is typically in the range of 2–10 pounds, although I have removed as much as 15 pounds. Liposuction will remove additional fat, usually several pounds. This makes a major difference in body contour, much more than a similar amount of weight loss from dieting. Obviously, in patients who are overweight, results are best from a combination of weight loss from dieting and surgery to correct body disproportions.
Q: How long before I can straighten up fully?
A: This depends on the degree of existing skin laxity, how low the incision is placed, and how much skin is removed. Ironically, lean patients with less skin laxity (but still enough to be of concern), who want the scar as low as possible to keep it concealed, will have the greatest abdominal tightness. These patients may take a couple of weeks to straighten fully. Most patients take about a week before they can stand fully straight.
Q: It feels very tight. Should I be careful to avoid pulling on the incision?
A: Yes, especially during the first week. Avoid pulling too much because this may place too much tension on the incision. After a week, you can stretch a little more. The key is to do a little more each day. Your body is a good guide and will tell you when to back off.
Q: When can I return to exercising?
A: You won’t feel like exercising after surgery. You can start walking a mile or 2 in about 2 weeks and return to exercising a month after surgery. Abdominal exercises will take longer, about 6 weeks at a minimum.