INTRODUCTION
In my practice, I perform only gender-affirming top surgery (I don’t perform the bottom
surgery), either female-to-male, or male-to-female. FTM patients are typically quite young, often
teenagers or in their early 20s. They have already been psychologically evaluated and started on
hormone therapy. Some patients identify as nonbinary rather than transgender. These patients
typically are not taking testosterone.
These patients wish to remove unwanted breast tissue. Typically, they spend time every day
wrapping the breasts and using binders. They are very self-conscious about this part of their
anatomy that is not consistent with their self-image. Fortunately, surgery can correct this
problem. Most patients are comfortable with their shirt off after surgery. Patient satisfaction
tends to be very high.
THE IMPORTANCE OF NIPPLE PRESERVATION
The nipple is a unique body part. I place high importance of preserving the nipple intact as
opposed to grafting it. A grafted nipple tends to look artificial. It is flat. There is usually little or
no sensation in a grafted nipple, and no erogenous (erotic) sensation. Pigmentation may be lost,
at least temporarily. The erectile function is lost. Nipple reconstruction can never truly duplicate
a nipple.
Even if the patient does not really care much about nipple sensation, permanent numbness is not
welcome, as anyone who has had a dental procedure can attest. Also there may be chronic
neuropathic pain as a result of division of the important nerves that go to the nipples.
“DOUBLE INCISION FREE NIPPLE GRAFT” – an operation that is best avoided
Today, many surgeons perform a “double-incision free nipple graft” procedure on transgender
and nonbinary patients. This description leaves out the word “mastectomy.” This is really a
breast amputation, leaving a long horizontal scar across the chest. This scar is hard to conceal.
Hypertrophy of the scar and “dog ears” (puckering at the ends of the scars) are frequent. The
grafted nipple often sits too high. The chest may be too flat. Most patients are still uncomfortable
with their shirt off after this procedure. I never use this operation.
In 2024, I conducted a retrospective outcome study on my gynecomastia and FTM gender-
affirming top surgery patients. This study challenges the conventional practice of large excisions,
long scars, and grafted nipples. This study has been submitted for publication.
My approach has many advantages – nipple preservation, fewer complications, fewer revisions,
and greater patient satisfaction with their chest appearance without a shirt on.
PHOTOS OF PATIENTS WITH - GENDER AFFIRMING TOP SURGERY
L.E., Age 18
Procedure: Direct breast tissue excision and liposuction of breasts. breast tissue removal in 2 sessions, combining liposuction and direct breast tissue excision.
Before, 3 months after 2nd operation

N.B., Age 20
Procedure: Direct breast tissue excision and breast liposuction.
Before, 4 months

L.J., Age 20
Procedure: Liposuction of chest and subcutaneous mastectomies.
Before, 4 months

D.K., Age 22
Procedure: Direct breast tissue excision and breast liposuction, liposuction of the abdomen and flanks.
Before, 3 months

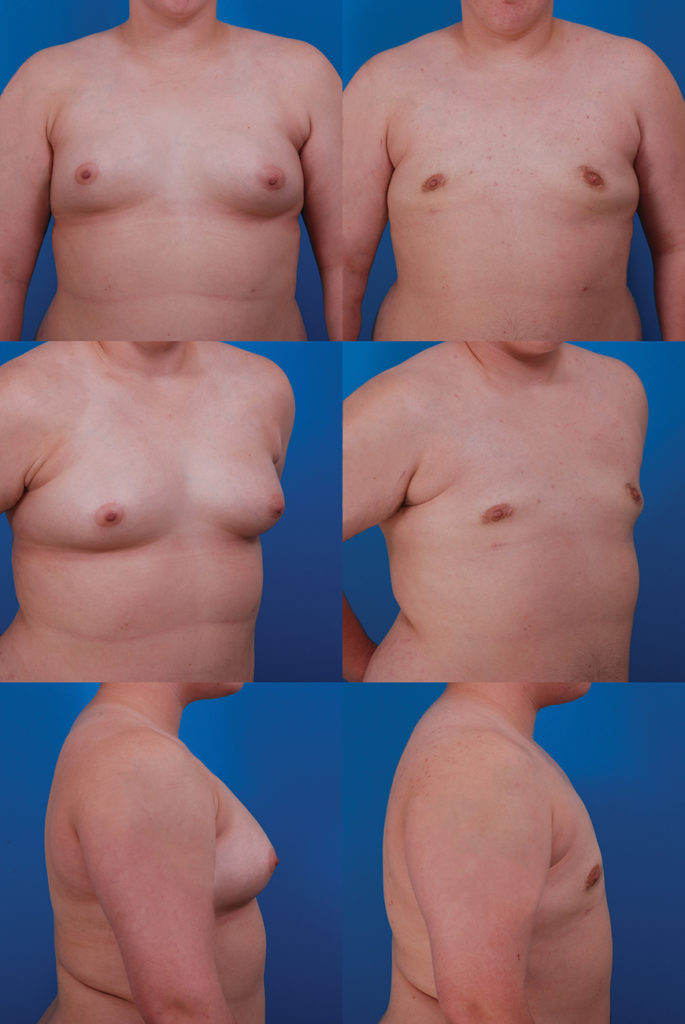
R.C., 26-year-old male transgender patient Top surgery using a vertical mammaplasty and nipple/areola preservation.
Second procedure: liposuction of the chest and scar revision.
Right breast: 1038 g
Left breast 1038 g
7 years postop.
SURGIC AL APPROACH WITH 100% NIPPLE PRESERVATION
My surgical approach is similar to treating gynecomastia in cisgender males. Because patients
are often young, skin contractility is usually quite good. This means that usually the breast tissue
may be removed without removing skin. The advantage is an inconspicuous scar that follows the
lower border of the areola. Even in patients with larger breasts, this is the usual approach. A later
procedure can be used to treat any skin excess that remains, keeping any scars to a minimum.
The nipple always remains attached. Preserving the nipple attachment is important for normal
nipple sensation and appearance.
Typically, the excess breast tissue is removed by direct excision (breast tissue is too firm to
remove by liposuction alone). In addition, liposuction may be used to remove fatty tissue. An
incision is placed in the crease below the breast for access. This small incision also serves as a
drainage site for the temporary suction drain. It is important to leave a cushion of breast tissue
under the nipple to avoid a saucer-like depression.
In patients with large, pendulous breasts, it is necessary to remove both breast tissue and skin. In
these patients, the nipple is still preserved intact. It is not grafted. The excess skin and breast
tissue is removed using a vertical (not horizontal) elliptical incision, often in combination with
an incision in the crease under the breast. The resulting scar does not extend onto the chest. The
scar is more hidden and less likely to develop scar healing problems such as hypertrophy or dog
ears. Patients may return at a later date for liposuction to achieve maximum flattening of the
chest, although some patients find a second procedure unnecessary.
Discomfort
Usually the pain is well-controlled with painkillers. If one side hurts more than the other, this
may signal a hematoma, which should be reported right away.
Drains
One drain is used for each breast. The drains are removed in the office 3 or 4 days after surgery.
When I include a vertical mammaplasty for patients with large, pendulous breasts, there is no
drain.
Hematoma
Because a pocket is created under the skin, a potential space is available for blood and fluid to
accumulate. A hematoma (blood collection) may develop despite the presence of a drain. This
usually happens within 24 hours of surgery. It is treated in the office with evacuation of the
hematoma.
Asymmetry
Contour irregularities are not unusual. These may respond to a touch-up liposuction or
sometimes additional breast tissue resection if they are quite noticeable. Perfect symmetry is
unrealistic.
Skin Folds
In patients with greater amounts of breast tissue, the skin may not contract adequately to avoid
skin folds. Such folds may be treated later with excision.
Scar Hypertrophy
Occasionally a hypertrophic scar may form that can be revised to make it less noticeable.
- A small amount of bloody drainage on the dressing is normal.
- The dressing is removed on the day after surgery. You can then bathe and shower when you return home. There are semitransparent adhesive tape (Steri-Strips) on the incisions. These tapes usually stay on for several days. If one is starting to peel off, go ahead and trim it or remove it. Avoid strenuous activities for 2 weeks after surgery. Avoid any heavy lifting for 2 weeks. This helps prevent excessive swelling.
- Drains are removed in the office in 3-4 days.
- Sutures come out in 1 week.
- Most patients are able to return to work within a week after surgery. If your work is physical you will require 2 weeks off.
- Strenuous exercise (examples: running, aerobics, tennis) should be avoided for 3 weeks. However, gentler exercise such as walking can be resumed 1 week after surgery. You may return to unrestricted activity 1 month after surgery. Your body will tell you—if your breasts are sore you are probably overdoing it.
- Once the tapes are removed, apply antibiotic ointment to the incisions, particularly any areas of crusting, twice daily. The crusts gradually come off on their own.
- Bruising is normal and usually goes away within a few weeks. It extends to the sides and abdomen because of gravity. Swelling is also to be expected and takes a month or two to resolve.
- Notify the office immediately if one breast appears to be getting much larger than the other. This could signal a hematoma, which requires prompt surgical attention.
- The compression garment with Velcro straps may be replaced with a less cumbersome garment that provides gentle compression of the chest, such as a tight-fitting athletic shirt (Under Armour is one brand). Usually this is done after the drains come out. The garment helps limit swelling, and most patients feel more comfortable wearing it. Most patients wear such a garment for 3-4 weeks and later while exercising.

