INTRODUCTION
Why Have a Breast Augmentation? PHOTOS OF BREAST AUGMENTATION
Studies show that one-third of all women are dissatisfied with the appearance of their natural breasts. Can a breast augmentation change this?
To better understand how well breast augmentation was meeting our patients’ expectations, we conducted a survey among 225 consecutive patients. Breast self-consciousness dropped from 86.2% to 12.6%. Remarkably, over 90% of women report an improvement in self-esteem after breast augmentation. No other cosmetic surgical procedure can match breast augmentation for patient satisfaction (98.1%). In our survey, the average result rating was 9.3 out of 10 on a scale of 1–10 and the median rating was 10, meaning that over half of patients scored their result a perfect 10 (!) and 98.7% of patients would do it again. (Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166.)
Breast augmentation with implants is arguably the most important advance in the history of cosmetic plastic surgery. It is also one of the most satisfying procedures for both the patient and surgeon in its almost magical ability to transform human shape. Gratification is almost immediate. It is an operation that reliably meets expectations (and exceeds them in almost half of patients). While rejuvenation of the face and body faces practical limitations, even older women can enjoy youthful looking breasts with the right combination of implants and lifts. No wonder this is a favorite procedure for cosmetic surgeons.
What Is the Ideal Breast?
What Is the Ideal Breast?
Smaller or larger? Full cleavage or subtle cleavage? Pendulous or perky? More fullness in the upper pole or the lower pole?
Among patients presenting for a breast augmentation, there is a consensus. Most women prefer more fullness in the top part of the breast. This is despite the fact that the normal breast typically is fuller in the lower pole. We should not be too surprised, in view of the purpose of bras and corsets before bras, meant to augment the upper poles of the breast. Few, if any, Greek statues portray a sagging or deflated breast!
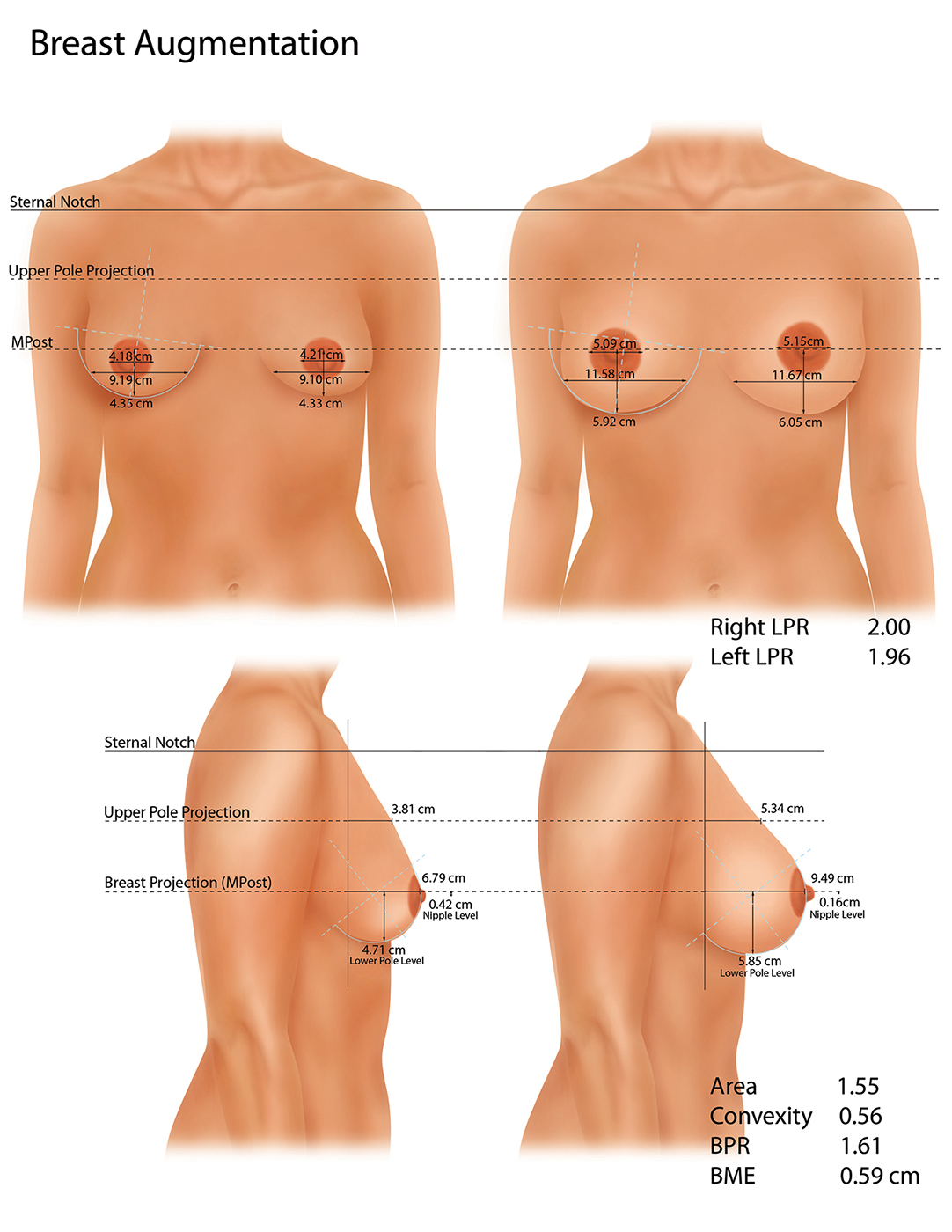
An upper pole/lower pole ratio of 45:55 (or 0.82) has been recently promoted in the plastic surgery literature (Mallucci P, Branford OA. Plast Reconstr Surg: 2014;134:436–447). This ratio calls for more fullness in the lower poles of the breasts than in the upper poles. Shaped implants are designed with this shape in mind. However, this ratio, 45:55, is also the same as the ratio among women choosing to have a breast lift, who have sagging breasts to start with. After breast augmentation, this ratio is closer to 1.6:1, and these patients report very high levels of satisfaction, 98.1%. Plastic surgeons need to remember that women desire ideal breasts, not necessarily natural-appearing ones (there being nothing more natural-looking that sagging breasts!).
- Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/mastopexy, and breast reduction. Plast Reconstr Surg. 2013;131:802e–819e.
- Swanson E. The ICE principle, 45:55 breast ratio, and 20-degree nipple inclination in breast augmentation. Plast Reconstr Surg. 2017;139:799e–801e.
What Is an Appropriate Breast Size?
Most women prefer larger breast sizes over smaller sizes. Of course, too much of anything can be detrimental, by definition, and very large breasts are undesirable to most women. The desired breast shape is parabolic in the upper pole, the shape of an umbrella held forward, and semicircular in the lower pole. Loss of fullness in the upper pole and excessive sagging of the lower pole are common complaints and universal ones, regardless of age, race, or culture.
Plastic surgeons have, historically, often been conservative in their size recommendations, and many are reluctant to insert large implants (implants > 350 cc). There is a perception that such sizes increase the complication rate. However, outcome studies of my patients actually show a positive correlation between implant size and patient satisfaction, and no increased risk of complications. Today, my average implant size is just over 400 cc, and women choosing large sizes tend to be highly satisfied.
No plastic surgical procedure has received as much public attention, and scrutiny, as breast augmentation. Breast augmentation decreased in popularity in the early 1990s due to media attention regarding the safety of silicone gel implants, and the 1992 FDA decision to make silicone gel implants unavailable to women desiring cosmetic augmentation (but allowed back on the market in the United States in 2006). Breast augmentation has resumed its place as one of the most popular cosmetic procedures today.
The procedure is not perfect and there are problems. However, even when complications are encountered, almost all women are still satisfied with their decision to have the procedure and would do it again. Fortunately, provided there is excellent communication and trust between patient and surgeon, almost all complications can be managed successfully. Very few women decide to have their implants removed and not replaced. Some women decide to have their implants removed and a simultaneous breast lift. But even this situation is unusual. Most women of all ages will have replacement implants.
It is important for the surgeon to try his or her best to reach an acceptable outcome with implants because the alternative, “deflated” breasts, is unattractive. Excellent communication, trust, skill and patience are needed between patient and surgeon because revisions are not without risk, and several procedures may ultimately be required. Like a marriage, the patient-physician relationship is tested when there are problems.
The outcome is different from woman to woman depending on what tissue is there to start with. Human tissues are not like clay and this is the difference between a sculptor and a plastic surgeon. A plastic surgeon has to work within the limits of real materials (the nature of the skin, existing breast tissue, the shape of the chest, implants). Fortunately, there is a range of breast shapes that are aesthetically pleasing. A breast need not be perfect, and perhaps there is some advantage in not having every woman resemble a Barbie doll. Although gross asymmetry is distracting and unappealing, small differences are well-tolerated. Within general guidelines, such as appropriate nipple level on the breast mound, more upper pole fullness than lower, and a tight lower pole, various breast shapes, even slightly pendulous breasts, can be attractive.
Breast Augmentation—Usually a One-Way Ticket
Furthermore, most changes are one-way. There is simply no “back button” to get you back to where you were before. A breast augmentation creates irreversible changes by stretching the skin and breast tissue. However, the change is so pleasing that few patients would reconsider their decision. In our own survey, 98.7% of women would have the surgery again.
Fat Injection of the Breasts
Fat injection has been a valuable addition to our armamentarium in facial rejuvenation and body contouring, such as buttock augmentation. It makes sense to consider using our own fat for breast enlargement. Women ask, “doc, can you take it from here and just move it to here?”
In the past, the plastic surgery community frowned on fat injection for breast augmentation. However, there is little doubt that it works. The problem is that several treatments may be needed. Only limited increases in volume are possible with a single treatment. It is time-consuming, and there must be sufficient donor fat tissue available, which can be scarce in thin women. Patients after breast augmentation using fat may have calcifications and excessive firmness of their breasts. Women, especially thin women, may have contour irregularities from aggressive liposuction to harvest the fat from other areas.
Fat injection cannot duplicate the results of breast implants in restoring upper pole fullness. Implants tend to hold their shape and do not deform with time the way natural breast tissue does (I often tell patients, “The worst thing about breast implants is that they are not the same as breast tissue, and the best thing about breast implants is they are not the same as breast tissue.”) Fat injection of the breasts is likely to be more expensive than a single breast augmentation procedure. Fat injection would be a more popular treatment if the results from breast augmentation using implants were not so consistently satisfactory. I have found fat injection to be a useful technique to fill in small breast defects after lumpectomies or after breast reconstruction, but not for breast augmentation.
The Desire for Larger Breasts
The desire to have fuller breasts is quite understandable in view of the importance of the breast to a woman’s sense of femininity and attractiveness. To deny this is to deny the reality of female form and sexuality. Fortunately, we live in a time when it is possible to safely enlarge breasts, so that women with small breasts need not be at a social disadvantage. With breast implants an option since the mid-1960s, it is hard to imagine a time when this was not available for women who were under-endowed. We live in a time when the “playing field” can be leveled (or perhaps “unleveled”) so breast-challenged women can compete.
Women who come to see the plastic surgeon have done so after considerable reflection. There is an element of embarrassment coming to a plastic surgery office and disrobing. Women are already dealing with some guilt about considering such a self-indulgence. Often, they are thinking about how friends and family are going to react. In the back of the mind are horror stories they’ve read or heard about. It is a wonder they work up the nerve to come in at all! And, yet they do, which shows the strength of the emotional need. In the past, women have endured truly awful treatments, such as silicone injections that led to painful lumps (“granulomas”). This was the only option for women who were born just a decade or two too early or in a country without modern standards of practice.
Contrary to popular belief, most women are not having a breast augmentation to satisfy others. Our survey found that 89% of women are having the surgery for their own reasons, 11% for both themselves and an “other,” and less than 1% just for the “other.” And, it is not a snap decision—they have usually been thinking of it for years. On average, our patients have considered it for 5 years before having the surgery. Sometimes they have been saving for a long time, or waiting until the kids are off to college and they feel they can reward themselves. I am reassured by consistently hearing women tell me that their husbands are supportive, but in most cases, not pressuring them to do it— “He loves me whether I do it or not. But, if I want to do it, he’s all for it.” Of course, the procedure is such that both partners can enjoy the result. Usually, husbands sit quietly and a little timidly in the examining room. I have never heard a husband object to the concept of larger breasts.
- Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166
What Happens to My Nipple Sensation After Breast Implants?
Surveys show that nipple sensation is important sexually to 80% of women. Of course, even if this is not the case, sensate body parts are always to be preferred. Sometimes I see women in my office who have had breast implants elsewhere who report that their only disappointment was in losing nipple feeling on one or both sides. They are usually still happy with their decision, but would be happier if they kept full nipple sensation! Sometimes nipple sensation does not get the attention it should from plastic surgeons.
A major sensory nerve supplies the nipple with feeling. This nerve is called the lateral cutaneous branch of the fourth intercostal nerve, and it comes from the side of the rib cage. It is at risk when the surgeon dissects the pocket for the breast implant. Some surgeons advocate making this pocket using cautery or a scalpel. Other surgeons, myself included, prefer to make the pocket bluntly, using our fingers. The advantage is that the nerve can often be felt and preserved intact. It might get stretched, but is unlikely to be cut. A stretched nerve will usually recover, but a cut nerve will not. This approach appears to be successful. Our survey revealed that only 2.3% of women experienced persistent nipple numbness.
This rate compares with a range of 12–20% in other series.
- Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166
Common Reasons Women Choose Breast Augmentation
Of course, like other areas of cosmetic surgery, I see women who are newly single due to a marital breakup or death. They are “back on the market.” Women who are divorced, and whose bodies have suffered the effects of childbirth, want to look as attractive as possible, mainly for their own sense of confidence. They are working out, toning their bodies, and this is just one of the self-improvement items on their list.
Some women do not want to have their partner’s attention wandering. One patient told me, “I was at the racetrack with my boyfriend, and there was no denying that full-chested women caught his eye. I just don’t want to have to deal with it.”
Breast Appreciation
A breast augmentation typically improves a woman’s sense of femininity, which can boost her own feelings of sexuality. Although the priority for most women is an improved body image, almost half report a positive effect on their romantic life. Their breasts are no longer a source of feelings of inadequacy, but a source of feminine pride and enjoyment. One patient told me after her breast augmentation, “This is how a woman is supposed to look.” It is an appreciation she experiences every day, looking in the mirror, putting on clothing, shopping for clothing, wearing an evening gown, and fitting a bathing suit.
High Patient Satisfaction
Partly by the process of financial selection, women tend to be in their 20s by the time they arrive in the plastic surgery office. These young women are generally not in a high income category. They are making a sacrifice to have this surgery. It is a sacrifice not to be taken lightly by the surgeon. For many young women, the first question is: “How much does it cost?” A few hundred dollars makes a difference.
I often ask patients after surgery “Are you glad you did it?” Of course, they are being put on the spot by their plastic surgeon, but I can tell from their spontaneity and enthusiasm and lack of hesitation in their response that they feel it was worth it. The psychological benefit they will enjoy every day and for years to come compares favorably to discretionary income spent elsewhere.
Older Women
Women over 50 sometimes ask if they’re too old for a breast augmentation. Of course, there is no real age limit and the results of breast augmentation are appreciated by patients of all ages. In fact, our capabilities of breast rejuvenation, which may include a breast lift in patients with sagging, compare favorably to results from other body contouring surgery, where we often have to settle for skin laxity and cellulite that cannot be completely corrected using presently available techniques. We may as well take advantage of superior results where we can get them! Youthful looking breasts can help compensate for aging elsewhere.
Breast Asymmetry
About half of women who present for breast augmentation have breasts that are asymmetrical in size and about half have nipples that are at different levels. Including asymmetry in the shape of the chest, nipple/areola size, and level of the crease under the breast, 88% of women have asymmetrical breasts before surgery! Women are often unaware how common this is. We have all seen women’s breasts portrayed in the visual media in various poses and amount of cover. But, most of us are not in the habit of critically inspecting large numbers of naked, unretouched women’s breasts. And, I am at a loss to think of anybody who is in such a habit, apart from a medical doctor or mammographer!
As part of the examination, plastic surgeons look for asymmetry before surgery. One reason we do this is to bring any existing asymmetry to the patient’s attention. She may have never noticed it before. But, she will look more closely at her breasts after surgery and, unless she knows about it beforehand, she may notice for the first time that one nipple is slightly lower or higher, or points outward more, than the other.
Nipples naturally point slightly outward because of the curved contour of the chest. A breast augmentation will not change this. It will not alter nipple placement on the skin. Sometimes, an optical illusion is created after surgery by the low position of the nipple on the breast mound—it appears that the implant is too high, when in fact the implant is correctly positioned on the chest, but the nipple is too low. Patients wonder, “Can’t you just put the implant lower?” But to lower the implant in such a situation, would make the whole breast appear too low. It would sit lower on the chest, look unnatural and would displace the natural crease under the breast (“inframammary fold”) downward. The implant has to be in the right position for the breast, not for the nipple. The logical way to correct a lowered nipple position is to elevate the nipple with the saggy lower breast tissue, and a breast lift is the operation that does this.
Women cannot expect breast implants alone to significantly raise the nipple position. Implants do not take up enough of the slack to really elevate the nipple. Our measurement study showed that the nipple is elevated only a few millimeters on average after a breast augmentation with implants. Women who have low-set nipples are best served with a breast lift at the same time.
- Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/mastopexy, and breast reduction. Plast Reconstr Surg. 2013;131:802e–819e.
Reducing Size Asymmetry by Adjusting Implant Volumes
The final breast volume represents a combination of the breast tissue that is there to start with plus the implant, which explains why two women with the same size implants may have different breast sizes. The implant simply fills out the breast envelope, so that characteristics of the breast (amount of existing breast tissue, nipple size and position) remain unchanged. With saline-filled implants, size asymmetry may be reduced by simply adding more fluid, or using a slightly larger implant, or both, on the smaller side. The prevalence of existing volume asymmetry explains why the implant volumes are often not identical in the patients shown in this section. Of course, any small size discrepancy is minimized anyway as the volume of both breasts is increased by the presence of the implants.
Silicone gel implants come already prefilled, so that very minor size adjustments are not possible. However, in patients who have noticeable size asymmetry, two different sized implants are used.
Perfect symmetry is virtually impossible and, fortunately, unnecessary to get an ideal result.
In patients with greater degrees of asymmetry, the breast “envelope” is tighter on the smaller breast and looser on the larger one. The nipple on the larger breast is lower and the areola is usually larger, because the nipple and areola are part of the same expanded ectodermal appendage that forms the breast. We need to use a larger implant on the smaller side to reduce the size discrepancy. Ideally, we would like to take up the slack more on the larger side, which tends to be saggier, but we have to use a smaller implant on the larger side (so this side does not end up too big), so the nipple will remain lower on the larger side. In this situation, a simultaneous breast lift is the better option. This way, the breast envelope can be tightened as necessary. The nipples can be more symmetrically placed at the same level and the areolae can be reduced to provide a better match.
In most cases, however, a mild degree of asymmetry does not bother women enough to have the additional scars that come with a breast lift. It is unusual for me to perform a breast lift on just one side. Usually, it is better to do it on both breasts. The breasts and nipples appear more symmetrical this way, because a lifted nipple looks different from a natural one. The border of the areola, which has been incised with a scalpel, is more distinct than a natural areolar border. It does not fade away into the surrounding skin like a natural areola. Better to have matching areolae. Additionally, many women, whose nipple is low enough on one side to justify a breast lift, benefit from having both breasts lifted anyway because even the smaller breast is a little saggy.
PATIENT PHOTOS, LISTED SMALLER TO LARGER IMPLANTS

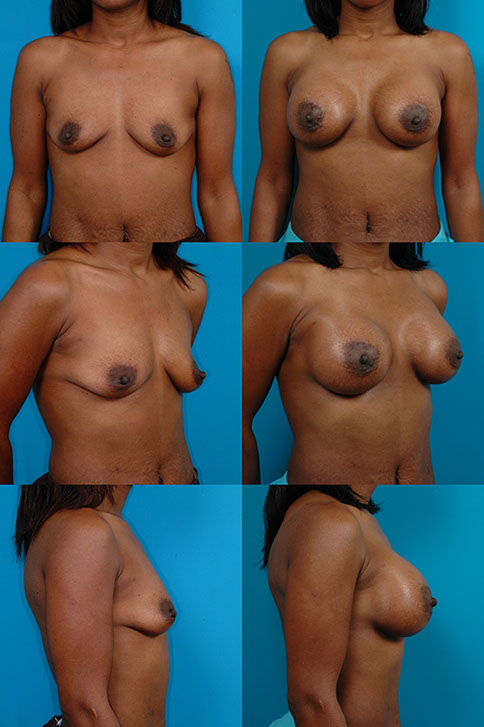
L.C. Age 28 Height: 5’4″ Weight: 129 lbs. Implant Size: 300cc Placement: Submuscular Approach: Inframammary 3 Months
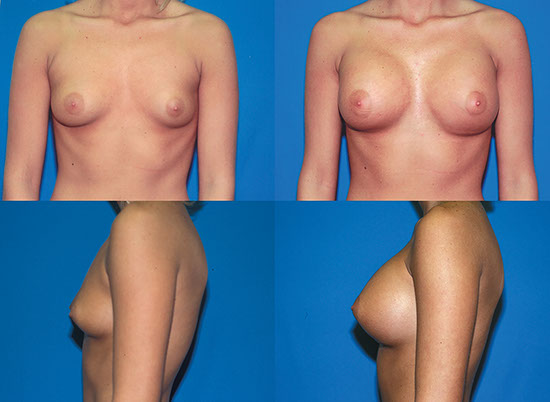
L.B. Age 28 Height: 5’4″ Weight: 123 lbs. Incision: Periareolar Placement: Submuscular Implant Size: 350cc

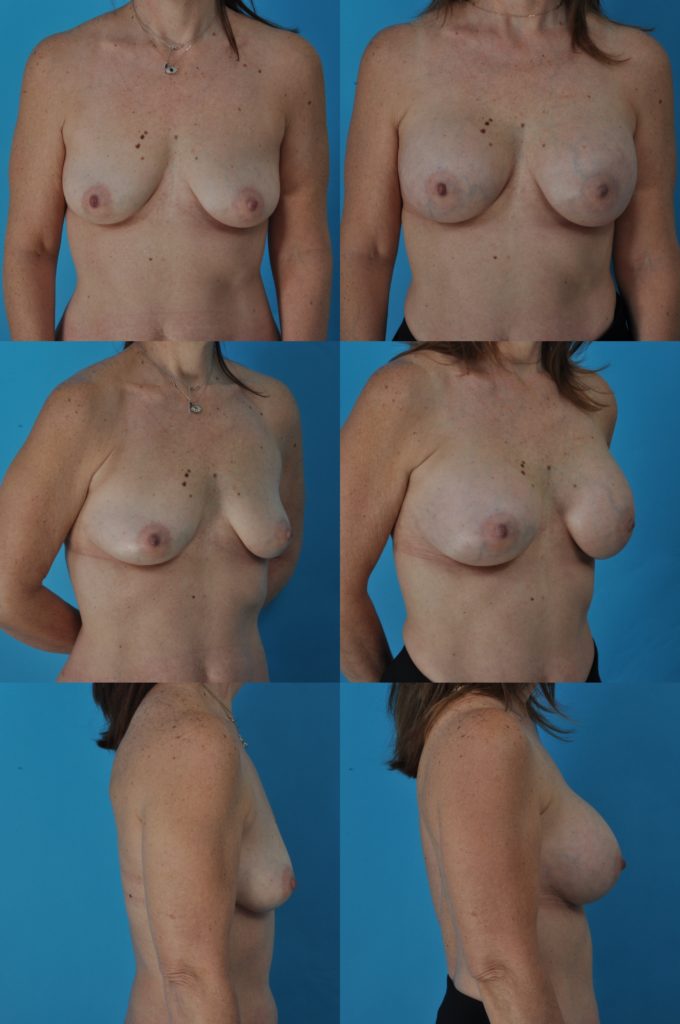
J.R. Age 36 Height: 5’6″ Weight: 133 lbs. Implant Size: 360 cc Placement: Submuscular Approach: Inframammary 2 Months After 2nd Procedure

V.A. Age 43 Height: 5’3″ Weight: 136 lbs. Implant Size: 360 cc Placement: Submuscular Approach: Inframammary Note: Also had a nipple reduction procedure. 3 Months After

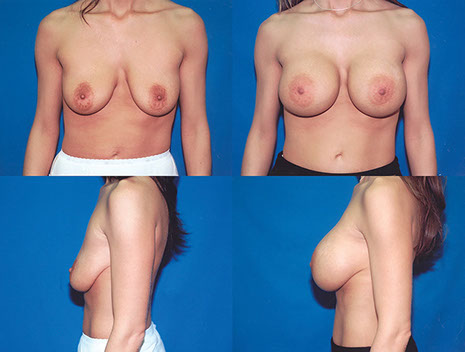
C.S. Age 34 Implant Size: 375 cc Placement: Submuscular Approach: Inframammary 1 Month
T.A. Age 27 Height: 5’1″ Weight: 110 lbs. Implant Size: 385cc Placement: Submuscular Approach: Inframammary 3 Months

M.V. Age 45 Height: 5’3″ Weight: 125 lbs. Implant Size: 397 cc Placement: Submuscular Approach: Inframammary 5 Years

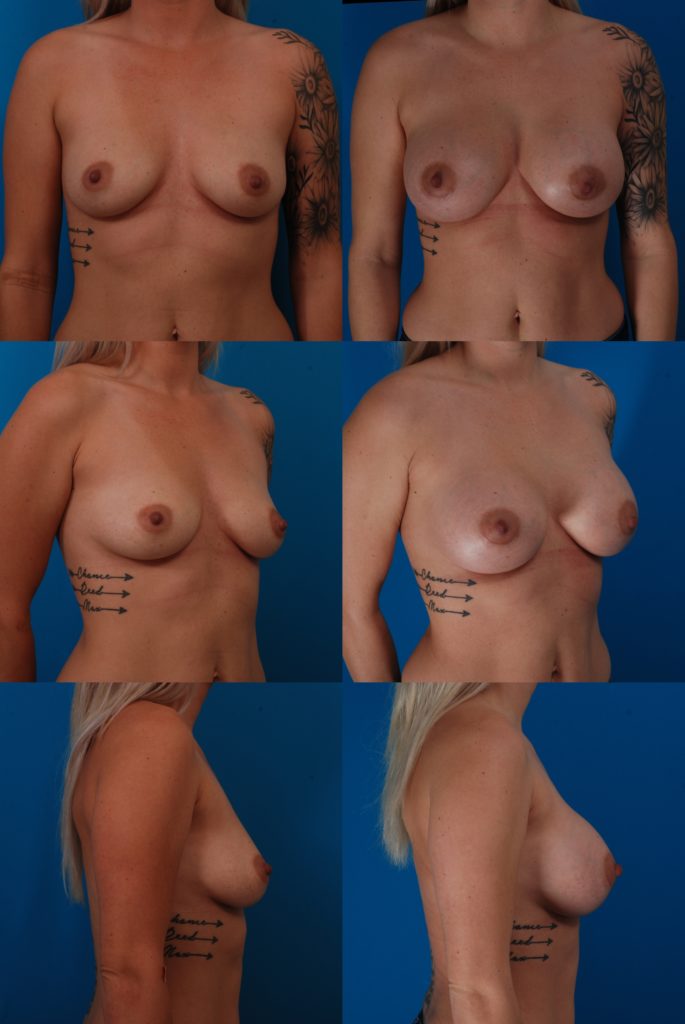
S.B. Age: 36 Implants: Right 400 cc, Left 425 cc Placement: Submuscular Approach: Inframammary 1 Month

A.C. Age 24 Height: 5’6″ Weight: 123 lbs. Implant Size: 400 cc Placement: Submuscular Approach: Inframammary 2 Months

S.M. Age 28 Height: 5’2″ Weight: 128 lbs. Incision: Periareolar Implant Size: Right Breast 425 cc/Left Breast 400 cc Placement: Submuscular 3 Years

Z.B. Age 24 Placement: Above the Muscle Implant Size: 415cc Note: This bodybuilder requested implant placement above the muscle 1 Month

K.H. Age: 27 Height: 5’3″ Weight: 121 lbs. Implant Size: 420cc Placement: Submuscular Approach: Inframammary 3 Weeks

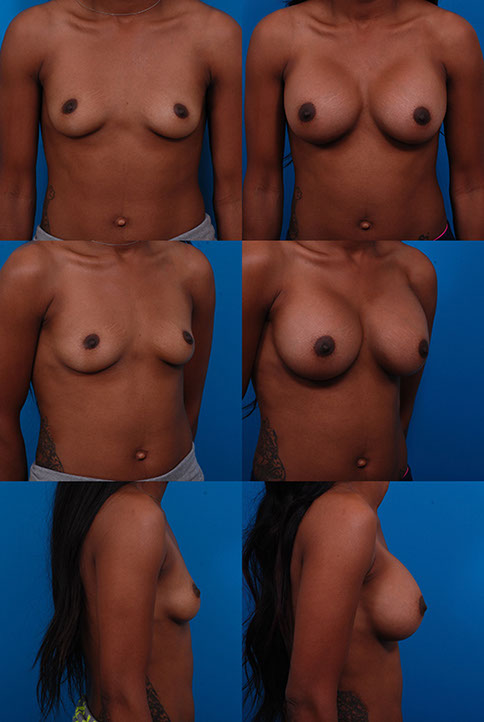
Q.J. Age 36 Implant Size: 425 cc Placement: Submuscular Approach: Inframammary 3 Month

J.L. Age 39 Height: 5’4″ Weight: 129 lbs. Implant Size: 425cc Placement: Submuscular Approach: Inframammary 3 Months
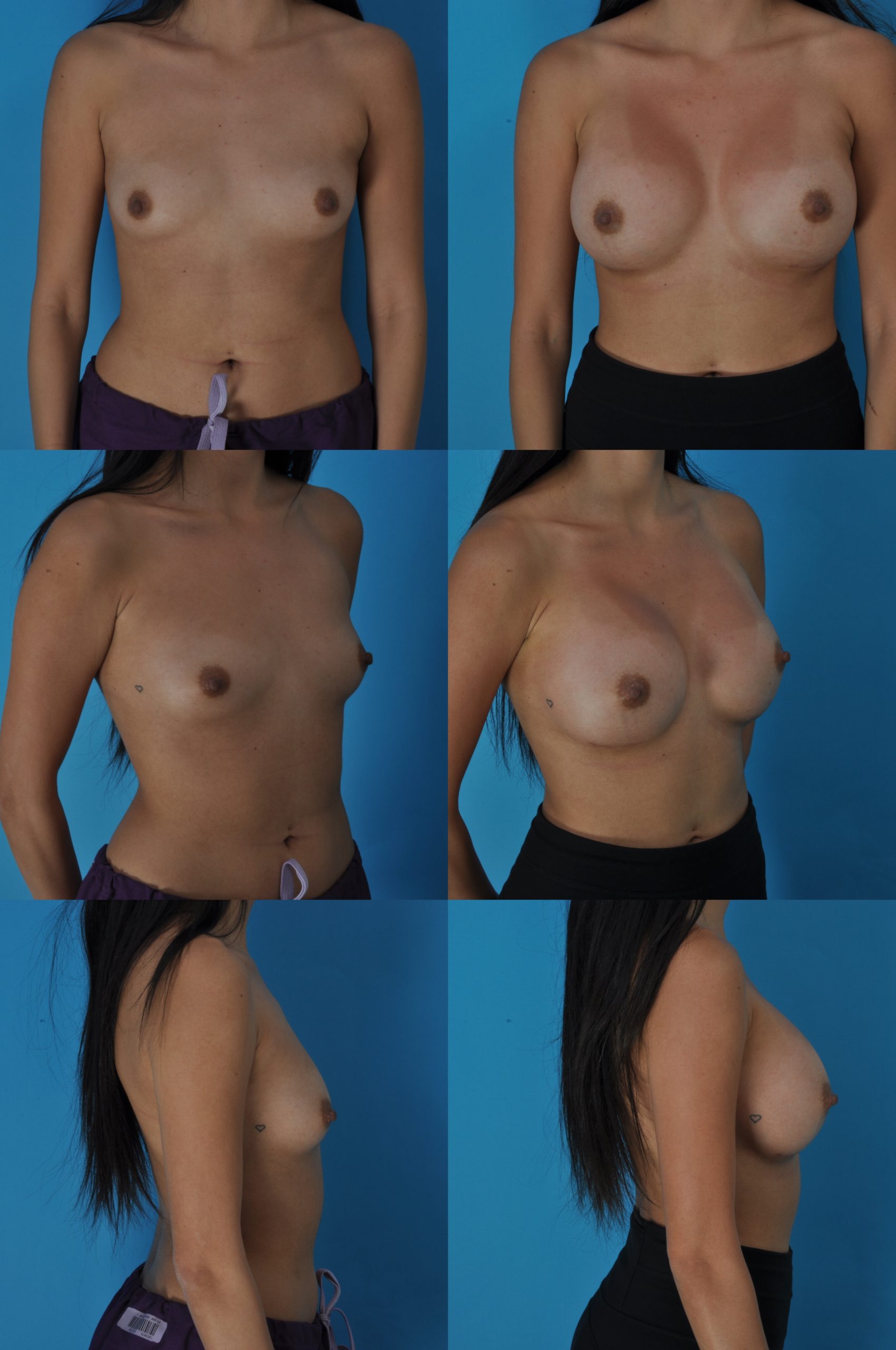
A.E. Age: 25 Height: 5’2″ Weight: 110 lbs. Implant Size: 450cc Placement: Submuscular Approach: Inframammary – 2 Months
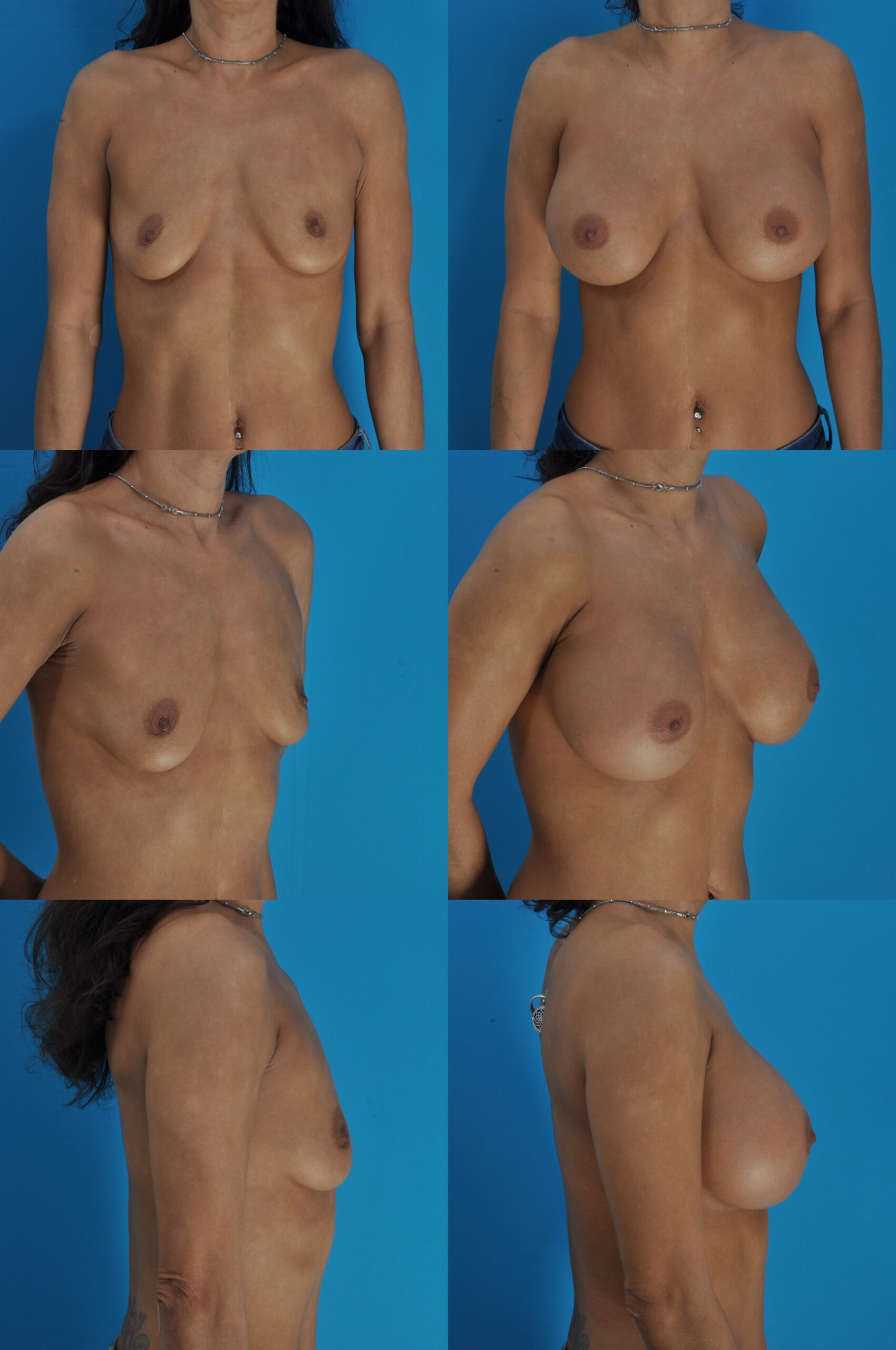
K.R. Age 41 Implants: 450 cc Placement: Submuscular Approach: Inframammary —– 3 Months

E.H. Age 27 Height: 5’5 Weight: 143 lbs. Placement: Submuscular Approach: Inframammary Implant Size: Right Breast: 500cc/Left Breast: 500cc 3 Months

A.B. Age 47 Implant Size: 500cc Placement: Submuscular Approach: Inframammary 3 Months

J.M. Age 25 Height: 5’3″ Weight: 136 lbs. Implant Size: 500cc Placement: Submuscular Approach: Inframammary 2 Years

Y.C. Age 27 Height: 5’1″ Weight: 105 lbs. Size: Right Breast: 500 cc/Left Breast: 510 cc Note: To improve symmetry, a right nipple elevation was done, using a “crescent” mastopexy to adjust the position of the right nipple and areola. The scar is still red and noticeable, but will fade over time. 2 Months

A.L. Age 35 Height: 5’3″ Weight: 114 lbs. Placement: Submuscular Approach: Inframammary Implant Size: Right Breast: 500 cc/Left Breast: 500 cc 3 Months

D.W.R. Age 23 Height: 5’4″ Weight: 168 lbs. Placement: Submuscular Approach: Inframammary Implant Size: Right Breast: 550 cc/Left Breast: 550 cc 3 Months

B.K. Age 28 Implant Size: 600cc Placement: Submuscular Approach: Inframammary 3 Months
A.G. Age 40 Height: 5’2″ Weight: 150 lbs. Implant Size: 600cc Placement: Submuscular Approach: Inframammary 3 Months

J.B. Age 22 and 29 Height: 5’3″ Weight: 120 lbs. Placement: Submuscular Incision: Inframammary Implant Size: (1) 360 cc, (2) 640 cc, 5 months after first augmentation (360 cc) and then 2½ months after replacement with larger implants (640 cc) 7 years later.

K.L. Age 29/41 Implant Size: 450cc replaced with 800cc Note: Patient had 2 procedures. 12 years/3 months

M.H. Age 19/28 420cc replaced with 800cc Note: Patient had 2 procedures 8 years/5 weeks
PHOTOS OF PATIENTS WITH A PERIAREOLAR INCISION
P.B., Age 23
Height: 5’3″
Weight: 105.5 lbs.
Implant Type: Mentor smooth, round, moderate profile, saline-filled
Placement: Submuscular
Approach: Periareolar
Implant Size: Right Breast: 330 cc/Left Breast: 325 cc
P.B. Age 23 Height: 5’3″ Weight: 105.5 lbs. Incision: Periareolar Implant Size: Right Breast: 330 cc/Left Breast: 325 cc

P.B. Age 23 Height: 5’3″ Weight: 105.5 lbs. Implant Size: Right Breast: 330 cc/Left Breast: 325 cc
L.B., Age 28
Height: 5’4″
Weight: 123 lbs.
Placement: Submuscular
Approach: Periareolar
Implant Size: Right Breast: 350 cc/Left Breast: 350 cc
Silicone Implants
L.B. Age 28 Height: 5’4″ Weight: 123 lbs. Incision: Periareolar Implant Size: 350cc
P.S., Age 30
Height: 5’4″
Weight: 115 lbs.
Placement: submuscular
Approach: Periareolar
Implant Size: 390cc
Saline Implants

P.S. Age 30 Height: 5’4″ Weight: 115 lbs. Incision: Periareolar Implant Size: 390cc
D.A. Age 33,
Height: 5’5″
Weight: 150.5 lbs.
Implant Type: Mentor smooth, round, moderate-plus profile, saline-filled
Placement: Submuscular
Approach: Periareolar
Implant Size: Right Breast: 400 cc/Left Breast: 420 cc
D.A. Age 33, Height: 5’5″ Weight: 150.5 lbs. Incision: Periareolar Implant Size: Right Breast: 400 cc/Left Breast: 420 cc
PHOTOS OF PATIENTS WITH COLLAPSED NIPPLE/AREOLAS
K.S., Age 41
Height: 5’9″
Weight: 158 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 440 cc/Left Breast: 450 cc
Saline Implants

K.S. Age 41 Height: 5’9″ Weight: 158 lbs. Implant Size: Right Breast: 440 cc/Left Breast: 450 cc
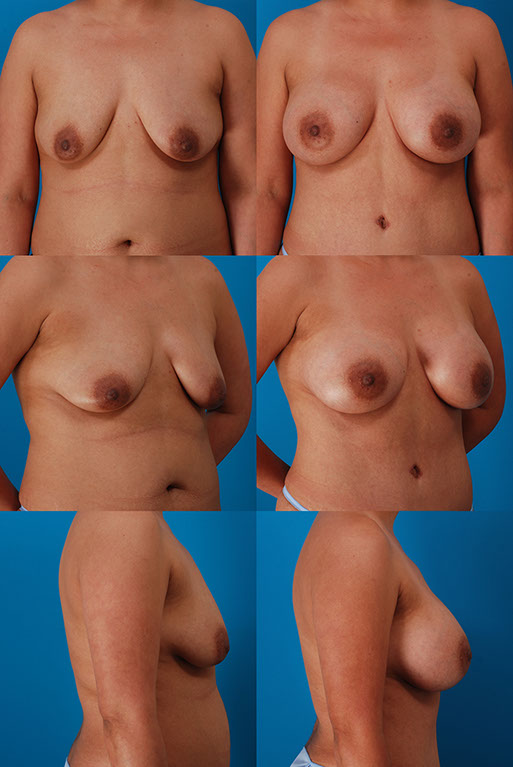
PHOTOS OF PATIENTS WITH TREATABLE ASYMMETRY
B.S., Age 20
Height: 5’8″
Weight: 126 lbs.
Implant Type: Mentor smooth, round, moderate profile, saline-filled
Placement: Submuscular
Incision: Inframammary
Implant Size: Right: 370 cc/Left: 425 cc
B.S. Age 20 Height: 5’8″ Weight: 126 lbs. Implant Size: Right: 370 cc/Left: 425 cc
Mild Asymmetry
K.E., Age 19
Height: 5’8″
Weight: 124 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 450 cc/Left Breast: 450 cc
Saline Implants

K.E. Age 19 Height: 5’8″ Weight: 124 lbs. Implant Size: 450cc
V.G., Age 19
Height: 5’7″
Weight: 156 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 450 cc/Left Breast: 450 cc
Saline Implants

V.G. Age 19 Height: 5’7″ Weight: 156 lbs. Implant Size: 450cc
A.D., Age 22
Height: 5’7″
Weight: 124 lbs
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 480 cc/Left Breast: 450 cc
Saline Implants

A.D. Age 22 Height: 5’7″ Weight: 124 lbs. Implant Size: Right Breast: 480 cc/Left Breast: 450 cc
J.D., Age 28
Height: 4’9″
Weight: 162 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 480 cc/Left Breast: 360 cc
Saline Implants

J.D. Age 28 Height: 4’9″ Weight: 162 lbs. Implant Size: Right Breast: 480 cc/Left Breast: 360 cc
T.B., Age 29.
Breast augmentation with right periareolar mastopexy and left vertical mastopexy. 3 months
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 520 cc/Left Breast: 550 cc
Saline Implants

T.B. Age 29. Implant Size: Right Breast: 520 cc/Left Breast: 550 cc Note: Breast augmentation with right periareolar mastopexy and left vertical mastopexy.
K.M., Age 32
Height: 5’6″
Weight: 125 lbs.
Implant Type: Allergan Natrelle smooth, round, moderate profile, saline-filled
Placement: Submuscular
Incision: Inframammary
Implant Size: Right Breast: 420 cc/Left Breast: 400 cc

K.M. Age 32 Height: 5’6″ Weight: 125 lbs. Implant Size: Right Breast: 420 cc/Left Breast: 400 cc
L.G., Age 32
Height: 5’1 “
Weight: 115 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 375 cc/Left Breast: 275 cc
Silicone Implants

L.G. Age 32 Height: 5’1 “ Weight: 115 lbs. Implant Size: Right Breast: 375 cc/Left Breast: 275 cc
PHOTOS OF PATIENTS OVER 50
M.C.
Age 52
Height:5 ‘2 “
Weight: 115 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast:300 cc/Left Breast:300 cc
Saline Implants
M.C. Age 52 Height: 5‘2“ Weight: 115 lbs. Implant Size: 300cc
C.M., Age 57
Height: 5’5 “
Weight: 140
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 550cc/Left Breast: 550cc Silicone

C.M. Age 57 Height: 5’5 “ Weight: 140 Implant Size: 550cc
PHOTOS OF PATIENTS WITH TUBEROUS AND NARROWLY BASED BREASTS
J.A., Age 27
Height: 5’7″
Weight: 143 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 420 cc/Left Breast: 420 cc
Silicone Implants

J.A. Age 27 Height: 5’7″ Weight: 143 lbs. Implant Size: 420cc
Before, 1 month after
S.G., Age 32
Height: 5’4″
Weight: 130 lbs.
Placement: Submuscular
Approach: Periareolar incision
Implant Size: Right Breast: 420 cc/Left Breast: 420 cc
Saline Implants

S.G. Age 32 Height: 5’4″ Weight: 130 lbs. Incision: Periareolar Implant Size: 420 cc
Before, 3 months, 7 years after
G.M., Age 29
Height: 5’7″
Weight: 142 lbs.
Implant Type: Mentor smooth, round, saline-filled.
Placement: Submuscular
Approach: Trans-Nipple
Implant Size: 400 cc

Before, 14 months after
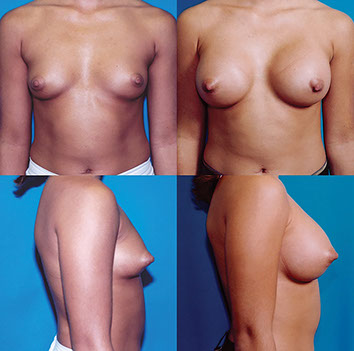
PHOTOS OF PATIENTS WITH SAGGING BREASTS TREATED WITH IMPLANTS ALONE

R.G. Age 30 Height: 5’7“ Weight: 142 lbs. Implant Size: 420cc Note: Sagging breasts treated with implants alone. 3 Months After
W.B. Age 30 Height: 5’4″ Weight: 114.5 lbs. Implant Size: Right Breast: 475 cc/Left Breast: 480 cc Note: Sagging breasts treated with implant alone. 10 Months After

B.N. Age 32 Implant Size: Right Breast: 470 cc / Left Breast: 480 cc Note: Sagging breasts treated with implant alone. 3 Months After
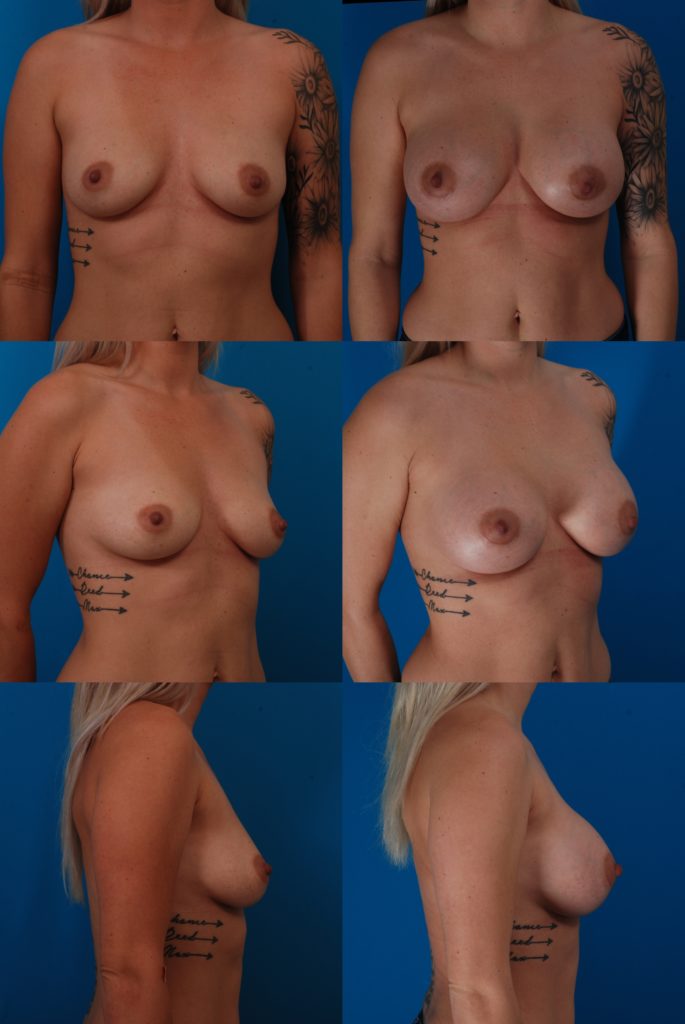
PHOTOS OF PATIENTS WITH IMPLANTS SETTLING OVER TIME
C.C., Age 30
Height: 5’5″
Weight: 116
Placement: Submuscular
Approach: Inframammary
Implant size: 450 cc
Implant type: Mentor smooth, round, moderate plus profile, saline-filled

C.C. Age 30 Height: 5’5″ Weight: 116 Implant size: 450 cc Note: Implants settling over time.
Before, 1 month, 3 months, 7½ years after
D.U., Age 33
Height: 5’6″
Weight: 131.5
Implant type: McGhan smooth, round, moderate-profile, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant size: 330 cc
D.U. Age 33 Height: 5’6″ Weight: 131.5 Implant size: 330 cc Note: Implants settling over time.
B.M., Age 33
Height: 5‘10½”
Weight: 141
Implant Type: Mentor smooth, round, moderate profile, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 400 cc
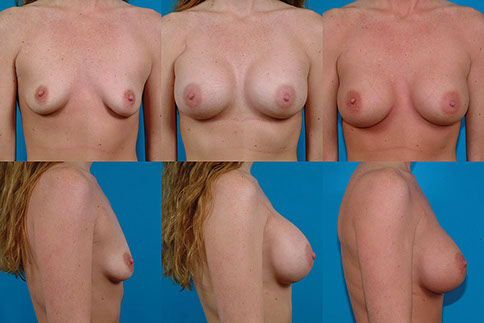
B.M. Age 33 Height: 5‘11” Weight: 141 Implant Size: 400 cc Note: Implants settling over time.
T.C., Age 34
Height: 5’3″
Weight: 124
Implant Type: Mentor smooth, round, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 400 cc

Before, 6 weeks after, 15 years after
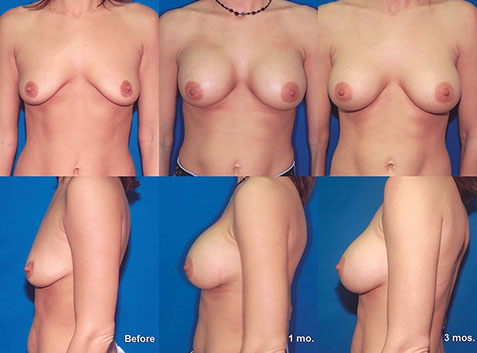
R.H., Age 43
Height: 5’4″
Weight: 130
Implant type: Mentor smooth, round, moderate-plus profile, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant size: 400 cc

Before, 1 month after, 3 months after
J.K., Age 26 and 36
Height: 5’5″
Implant Type: McGhan round, moderate profile, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 400 cc

Before, 6 weeks after, 10 years after
PHOTOS OF PATIENTS WITH INDIVIDUALIZED BREAST CONDITIONS
Pigeon Chest (“Pectus Carnae”)
C.B., Age 27
Procedure: Breast Augmentation
Height: 5’4″
Weight: 108 lbs.
Implant Type: McGhan round, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 375 cc

Before, 7 weeks after
Tuberous Breasts
G.M., Age 29
Height: 5’7″
Weight: 142 lbs.
Implant Type: Mentor smooth, round, saline-filled.
Placement: Submuscular
Approach: Trans-Nipple
Implant Size: 400 cc

Before, 14 months after
Sunken Chest (“Pectus Excavatum”)

Before, 6 weeks after
Stretch Marks
Women often ask if breast implants cause stretch marks. One would think that the tension created by inserting breast implants might cause stretch marks. Fortunately, implants themselves do not usually cause stretch marks.
In fact, we do not know why some women are prone to developing stretch marks after pregnancy or weight loss, or just by virtue of having larger breasts. Certainly there is a genetic predisposition. Whatever skin changes have occurred to cause the development of stretch marks in the past, or possibly will occur in the future, these changes seem to go on regardless of the presence of implants. Existing stretch marks are not improved by the augmentation, but they are not made worse either. The breasts look better anyway, and the stretch marks can be less obvious because the tone of the skin is improved by taking up the slack, making any contour depressions caused by stretch marks less visible.
J.V., Age 33
Height: 5’7″
Weight: 130 lbs.
Implant Type: McGhan, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 380 cc

Before, 1 year after
Collapsed Nipples
K.A., Age 35
Height: 5’0″
Weight: 103 lbs.
Implant Type: Mentor round, saline-filled
Placement: Submuscular
Approach: Inframammary
Implant Size: 300 cc

Before, 3 months after
Over projecting Nipples
J.V., Age 40
Height: 5’2″
Weight: 84 lbs.
Implant Type: Mentor smooth, round, moderate-plus profile, saline-filled
Placement: Submuscular
Approach: Trans-Nipple
Implant Size: 270 cc

Before, 3 months after

Close-up of incision
Inverted Nipples
H.C., Age 24
Height: 5’7″
Weight: 117 lbs.
Placement: Submuscular
Approach: Trans-Nipple
Implant Size: 380 cc
Implant Type: Mentor smooth, round, moderate profile, saline-filled

Before, 4 weeks after
PHOTOS OF PATIENTS THAT TRANSITION FROM MALE TO FEMALE
C.M., Age 23
Implant Type: (1) Saline-filled (2) Natrelle smooth, round high profile saline-filled
Placement: Submuscular
Incision: Inframammary
Implant Size: (1st procedure) 400 cc, (2nd procedure) 900 cc

Before, 1 month after the second operation
PHOTOS OF PATIENTS WITH REPAIR OF EXISTING DEFORMITIES AFTER PREVIOUS BREAST AUGMENTATION
A.G., Age 21
Procedure: Replacement of breast implants and capsular repairs. This patient had 2 previous breast augmentations previously, performed elsewhere. Her existing implants were replaced with a larger size and both capsules were released medially and superiorly and reinforced laterally and inferiorly.
Height: 5’7″
Weight: 135 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 457 cc/Left Breast: 457 cc
Silicone Implants

Before, 1 year after
A.W., Age 36
Procedure: Replacement of breast implants and capsular repairs. This patient had a previous breast augmentation performed elsewhere and a previous attempted correction of symmastia and bottoming out.
Height:5’6″
Weight: 148 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast:450 cc/Left Breast:450 cc
silicone Implants

Before, 3 months after
S.U., Age 37
Breast augmentation with lateral capsular repairs and removal of accessory nipple from left breast. This patient had a breast augmentation elsewhere 7 years previously.
Height:5’4″
Weight: 141 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast:600 cc/Left Breast:600 cc
Silicone High profile Implants

Before, 3 months after
L.D., Age 42
Revision of breast augmentation. This patient had a breast augmentation 7 months previously. Her left side showed bottoming out. The capsules on both sides were adjusted.
Height:5’7″
Weight: 144 lbs.
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 475cc/Left Breast: 475cc
Silicone Implants

Before, 7 months, 3 months after 2nd procedure
PHOTOS OF PATIENTS WITH REMOVAL OF BREAST IMPLANTS
J.W., Age 29
Procedure: Removal of breast implants. This patient wanted to have her implants removed because of personal preference. She ran a half marathon 3 weeks later.

Before, 1 month after
Today breast augmentation is done primarily in ambulatory surgery centers and in office operating suites. My patients have surgery at the Surgery Center of Leawood, an adjoining state-licensed ambulatory surgery center. All members of the American Society of Plastic Surgeons must use accredited facilities. This is an important safety consideration.
Anesthesia
You might have noticed that I place anesthesia right at the top of the list. Proper anesthesia is vital to patient safety. I prefer a total intravenous anesthetic. This form of anesthesia provides the ideal balance of patient comfort and safety. Patients are asleep for their surgery and wake up afterward with no recollection of the surgery. This type of general anesthesia differs from traditional general anesthesia in avoiding gas, intubation, paralysis, and mechanical ventilation. I call this type of anesthesia “SAFE” anesthesia. These letters stand for “Spontaneous breathing, Avoid gas, Face up, and Extremities mobile.
- (Swanson E. The case against chemoprophylaxis for venous thromboembolism prevention and the rationale for SAFE anesthesia. Plast Reconstr Surg Glob Open 2014;2:e160.)
Implant Placement: Under the Muscle
Surgeons tend to have a preference regarding implant placement and use the same approach in almost all of their patients. Most plastic surgeons today favor the submuscular approach. Submuscular placement of the implant is achieved by developing a pocket between the pectoral muscle above (superficial) and the rib cage below (deep). The pocket is under the muscle, which is under the breast tissue. The muscle is lifted off the chest wall, making a pocket underneath. Most of the dissection can be done with the surgeon’s fingers, which helps preserve a major nerve (lateral branch of the fourth intercostal) that provides feeling to the nipple. By using blunt finger dissection, it is possible to avoid cutting this nerve. Surgeons using other forms of dissection, such as cautery or a scalpel are theoretically more likely to damages these important sensory branches.
The creation of this pocket is the main source of variation from one surgeon to another. After all, the implant used by most plastic surgeons in the U.S. is likely to be similar. Only three manufacturers, Mentor, Allergan, and Sientra produce almost all the implants used by American plastic surgeons. The pectoral muscle is released just the right amount over the breastbone (“sternum”) to achieve cleavage.
With an inadequate release, the space between the breasts may be too wide, especially in thin women. Women often ask about this problem at their consultation. They’ve seen pictures in magazines showing a wide space between the breasts. There should not be a wide flat space between the breasts, contained by the inside borders of the breasts that appear to spring forward from the chest like bookends. Instead, the breasts should come together to provide a cleavage when a bra is worn. Without a bra, the breasts should settle apart naturally.
The pocket needs to be big enough to avoid wrinkling of the implant as it is filled, but not so big as to create an unnatural bridge between the breasts, due to overdissection of the pocket in the medially, in the area of the cleavage. This problem is called “synmastia” or “symmastia.” The breasts appear to run into each other, with inadequate separation, the opposite problem from the “bookend” look, and resembling buttocks.
The most important advantage of submuscular placement is a more natural appearance. Because most of the implant is covered by muscle, unnatural overly-defined borders of the breast are prevented. The “half grapefruit stuck to the chest look” is avoided. The test of a well-done breast augmentation is the appearance of the cleavage. The cleavage should be natural, without a distinct border to suggest the presence of an implant. Because implants placed deep to the muscle have an extra layer of muscle over them, they are more difficult to feel. This is particularly important in thin individuals, or older women who may have less fatty tissue to conceal the implants.
The risk of capsular contracture is reduced by submuscular placement. Mammograms are made slightly easier, because there is some separation between the breast tissue and the implant, except the lower outer corner, where the implant is not completely covered by muscle. Some surgeons call the submuscular placement a “dual-plane” technique, recognizing that the implant is submuscular only in the area covered by the pectoralis major. Therefore, it is partially under muscle and partially under breast tissue.
Any Disadvantages of Submuscular Placement?
Yes. The surgery is more painful than the above-muscle (also called “prepectoral” or “subglandular”) augmentation. In my experience, very few patients, on being informed of the merits of both techniques, elect to have an above-muscle augmentation. I use the submuscular placement in almost all of my patients. You may have noticed that all the patients featured in this section have submuscular implants. If a patient has existing implants above the muscle, her replacements are placed under the muscle if this is possible.
Some women develop “animation deformity” after a submuscular breast augmentation. When they contract their pectoralis muscle, the implant displaces. This problem can be minimized by releasing the muscle along its origin at the bottom of the sternum. Occasionally a patient asks for prepectoral placement, which avoids this issue. However, in my practice even bodybuilders and fitness enthusiasts usually opt for a submuscular implant placement.
Breast Size
The question of how large to make the breasts is on every patient’s mind at the time of consultation. Women often show me photos on their mobile devices to demonstrate what they have in mind. The pictures help me to know what size the patient has in mind.
Most women already understand that their breasts will not look identical to one of the models on their mobile device; they will retain many of their original breast characteristics such as general shape, nipple level and nipple position on the breast. Their breasts are simply filled out.
Women may have a certain volume in mind: “A girlfriend had 350 cc implants and she looks great!” Breast size is a highly personal decision. I try to help patients make this decision, based upon my own experience and judgment. It turns out though, that most women have similar desires—they want larger breasts, but not too big! Many women do not know for sure what size they want. This is uncharted territory and they don’t know yet how they are going to react. It is my job to listen to what they say and give them the benefit of my experience to help them reach the right decision.
(Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166.)
The surgeon needs to individualize according to the desires of the patient. If this is done, the vast majority of women are very happy with their breast size after surgery, and the likelihood that they will need another operation to adjust breast size is minimized. This is important, because a second operation roughly doubles the expense and risk of complications. It is also important to recognize that some women will inevitably change their minds about size after having implants and that is okay, too. The reoperation rate for a size change will never be zero.
Breast Augmentation and Cup Size
If a patient wants a B-cup, that’s okay and it is her choice, but I tell her she can move up slightly to a C-cup size and she will not regret it. The most commonly requested size is a size that sits on the cusp of a C and D-cup (some bras a C and some bras a D). Generally, this size provides an excellent appearance, and is not so large that the breasts interfere with activities or appear “top heavy.” Patients who desire a full cleavage should select a D-cup size. The B-cup will not allow for spontaneous cleavage, but cleavage may be obtained by wearing a push-up bra. Personally, I believe (and my patients tend to agree) that women should not have to wear a push-up bra or inserts in their bras after a breast augmentation. This is why I counsel patients who are thinking of a modest B-cup size to consider a C-cup. But the decision is theirs.
The vast majority of women in my practice are satisfied with their breast size after surgery and would not change it. If they were to change, it would usually be to a larger size. Patients almost never find that they are too big a month after surgery, when the swelling has gone down. If a patient is going to have second thoughts later about size, it is usually that she would like to be larger. If a patient is “on the fence” about a B or C size, or C versus full C size, I tell them to choose the slightly larger size. It is unlikely they will return saying they are too big. Tellingly, most women ask to have larger implants inserted if they have their existing implants replaced for a deflation.
Of course, the surgeon cannot guarantee a certain bra cup size after surgery and bras do tend to fit differently from one manufacturer to another. A patient may find she is a C-cup size in one bra and a D-cup in another.
Do You Make Measurements on My Breasts to Gauge Implant Size?
Size selection remains much more of an art than a science. There is no formula that will provide the correct size of implant. Plastic surgeons have published systems to calculate implant size based on chest measurements, but these measurements consistently produce modest volumes that most patients would consider too small.
Is It Helpful to Stuff My Bra with an Implant to Determine Size?
It is important to remember that an implant stuffed into a bra is different from an implant inserted behind the muscle in the breast. I do not find this method very helpful in size selection.
Breast Tissue + Implant Volume = Breast Size.
Final breast size depends not only on the implant size, but also on how much breast tissue is there to begin with. A woman who desires a full C-cup size and is presently a small B-cup will require a smaller implant than a woman starting from an A-cup size. In viewing the before and after pictures of the Breast Augmentation section, it is obvious that the preoperative breast size is as important as the implant size in determining the final breast size. The elasticity of the skin also makes a difference.
Is 3-D Computer Simulation Useful?
Some surgeons use three-dimensional photographic systems in their office and computer simulations. It is important for women to know that these simulations are inaccurate because the software is not based on measured changes in breast dimensions. At present, this technique remains a marketing strategy. Proponents claim that it increases their “conversion rate,” which is a marketing concern, not a scientific one.
The Incision
There are three common approaches to place the implant. An incision may be made in the crease under the breast, along the edge of the areola, or in the armpit. Occasionally I insert the implant through a trans-nipple incision, particularly when I am correcting an inverted or overly projecting nipple simultaneously. Few plastic surgeons use the umbilical approach because it is impossible to place the implant submuscularly using the trans-umbilical approach.
The Inframammary Incision
The most common approach for breast augmentation is the inframammary incision located on the lower part of the breast, just above the crease under the breast. This way, the scar is hidden even if the bikini top slides up slightly. Frequently I see women who have had past augmentations using an incision placed exactly in the crease under the breast. In this location, there may be some friction on the incision from the bra strap after surgery, and the scar may end up being more conspicuous. At least one NFL cheerleader has exposed such scars when lifting her arms above her head!
The properly-placed inframammary incision allows women to wear a bikini or evening gown with concealment of the scar. Importantly, this placement of the incision also allows the surgeon optimal exposure to create the pocket where the implant is to be inserted. This ease of approach is important because the shape of the breast and the quality of the cleavage are the most important criteria in getting an ideal result, even more important than the incision. A short scar in the crease under the breast is inconsequential.
My incision placement is usually just above the existing inframammary crease, called a “supra-IMF” incision, to keep it extra well-hidden and avoid any rubbing from the bra. The inframammary ligaments are preserved to reduce the risk of bottoming out of the implant.
- Swanson E. The supra-inframammary fold (supra-IMF) approach to breast augmentation: Avoiding a double bubble. Plast Reconstr Surg Glob Open 2017;5:e1411.
The Periareolar Incision
The periareolar incision makes use of the natural border around the areola to hide the scar. It is a very acceptable alternative to the inframammary incision. The scar may be more visible here along the edge of the areola, particularly if the patient happens to be a poor scar-former, than it would be tucked on the underside of the breast. Nevertheless, if a patient requests this incision, I am hppy to oblige and the scar tends to be inconspicuous.
The Transaxillary Incision
Although the armpit approach has the advantage of avoiding incisions on the breast, it does leave a scar in the armpit. Usually this scar heals well and is inconspicuous. However, it may be visible if the patient raises her arm while in a bathing suit or evening gown. A few patients have told me they knew their hairdresser had implants because they could see the armpit scar. It is more difficult to dissect the breast pocket because the incision is more removed from the area of dissection. If subsequent breast surgery is performed, for example, an open capsulotomy to release a capsular contracture, an inframammary incision is used, so now the patient has two scars on each side rather than one. There may be some disadvantage to a transaxillary approach if the patient needs lymph node sampling at a later time as part of breast cancer treatment.This approach is rarely used by plastic surgeons today.
The Importance of Skill and Experience
Of course, most plastic surgeons (who are not as a group ego-challenged) have their own idea about results and it is not enough that a patient merely be satisfied. What can separate an ideal breast augmentation from a merely acceptable one is the skill and experience of the surgeon in creating the pocket for the implant—how much to release the muscle, making the implant pocket the right size and the correct position. Other matters of a technical nature—the particular approach used, the type of implant selected, and postoperative preferences are less important than the surgeons’ skill in correctly creating the pocket.
Experienced and skilled surgeons consistently produce satisfying results by learning through experience (good and bad, but mainly bad). Their reoperation rate drops as they advance along the learning curve. They learn how to properly create the pocket to achieve the most natural-looking result. Others may wonder but not know if a woman has had implants—has she or hasn’t she?
It is vital to place the implants at the correct level. Otherwise, the breast mounds will be unnaturally high (the busting-out look), or too low, a common problem seen in nude centerfold models whose implants have settled too low, pushing down the natural crease under the breast (inframammary fold) so that the nipples appear to be riding high. In making the pocket, the experienced surgeon takes settling of the implants due to gravity into consideration. Implants that appear correctly positioned immediately after surgery will, in time, appear bottomed out. For this reason, it is important for patients and surgeons to look at their long-term results. Implants that are placed correctly may appear to be too high for the first few months after surgery, until they settle into their proper position. Patients are therefore cautioned to expect that their implants will look too high at first, a little too perky. Being a little overly perky at first does not pose a problem. The appearance is certainly not objectionable in clothing.
Silicone Gel-Filled vs. Saline-Filled Breast Implants
Both silicone gel-filled implants (“silicone gel” implants) and saline-filled implants (“saline” implants) have silicone envelopes. The envelopes are made of a hard (“polymerized”) form of silicone that has a firm consistency, like rubber. This material breaks down in our bodies in only very minute quantities, in fact less than our environmental exposure to silicone from such household products as antacids and deodorants. Implants in the body such as pacemakers, catheters, and artificial joints have been coated in this inert material for decades. It is a tried-and-true material that is safe. It is doubtful that anyone is allergic to it, or rejects it.
Silicone gel-filled implants contain the gel form of silicone. This material is gelatinous, with the consistency of jelly. It is soft and squishy. This characteristic is desirable and one reason that silicone gel was chosen as a filler for breast implants in the first place.
Saline-filled implants, on the other hand, have a similar envelope made of the hard form of silicone, but are filled with salt water (“saline”), which is known to be completely safe, with a salt concentration similar to our body fluids. But, the implant is not as squishy and soft. A saline-filled implant is firmer. It feels more like a water balloon. The softer feel of a silicone gel implant is its advantage.
Many patients find the safety of saline reassuring. They are concerned about having silicone gel implants in their bodies, with some degree of leakage of silicone into the tissues over time, however minimal, and the possibility of undetected implant rupture. This issue is more important to them than the advantage in consistency of silicone gel implants.
It is important to note that if a capsular contracture develops (a tightening of the capsule around the implant), both types of implants will feel overly firm.
Frequently, the difference in feel characteristics of the two types of implants is a moot point. Women with a moderate amount of breast tissue to start with, for example, a B-cup size, notice less difference in consistency between a saline implant and a silicone gel implant because there is proportionately more breast tissue to feel. Also, most of these women do not mind a little additional firmness because they feel their tissues are too loose to start with.
In women who are very thin or have virtually no breast tissue, the feel difference between the two implant styles is likely to be greater, because there is proportionately less natural breast tissue, so that the consistency of their breast is virtually the same as the consistency of the breast implant. Also, there is slightly less risk of wrinkling with silicone gel implants (but it can still happen). In these thin patients, the risk-benefit ratio may favor silicone gel implants. Silicone gel implants are more expensive than saline implants. They also require a slightly longer incision and therefore a longer scar, because they come pre-filled.
Detection of Implant Deflation
The detection of deflation is not a difficult diagnostic issue for saline implants. The breast volume deflates over a period of hours or days. Clinical detection is straightforward. The breast just seems to deflate. There is no harm because the saline fluid is absorbed by the body and is harmless. But the implant needed to be replaced to restore symmetry.
A leaky silicone gel implant is difficult or impossible to detect just by examining the breast. The breast does not simply deflate the way it does when a saline implant leaks and the water is absorbed by the body. Instead, the viscous silicone gel is held in its pocket by the capsule that forms around the implant.
Safety of Silicone Gel Implants
Most of us (okay, maybe just those of a certain age) are aware of the concerns about silicone gel breast implants, which were impossible to miss in the media in the early 1990s. These reports highlighted “local” problems with breast implants that occur in the area of the breasts—mainly implant leakage and capsular contracture. There were also concerns that silicone may be causing health problems in other parts of the body. The debates were very emotionally-charged. Fortunately, evidence from large reputable studies, including one from the National Institute of Health, published in the reputable New England Journal of Medicine, showed that there is no increased risk of autoimmune diseases or breast cancer in women with breast implants. This is an important finding because some people had suspected that silicone from the implants might cause the body to start producing antibodies that might go on to attack normal tissues, such as the joints for example. Such autoimmune diseases as rheumatoid arthritis, lupus, and scleroderma do happen in women with breast implants. But these diseases also happen in women without implants. There is no evidence of one causing the other—scientists say there is no causal relationship. When these diseases occur in women with implants, it is a not-unexpected coincidence. Studies show the same is true for breast cancer.
What Happens When a Silicone Gel Implant Leaks?
Most of the time, the patient notices no change. There may or may not be a change in shape or size of the breast. Why not? Because the gel, which is a gelatinous material like Jell-O, is walled off by the capsule that the body forms around any artificial device that is inserted in the body. The silicone gel tends to stay in this pocket, so it is usually impossible to tell by examining the breast whether or not the implant is still intact. It is even difficult to tell on a mammogram, because silicone gel looks the same whether it is inside or outside the envelope, which it too thin to see on the mammogram. MRIs are more reliable for detecting implant rupture.
“Gummy Bear” Implants – Now Obsolete
There is a type of breast implant, which has been available in Europe and Canada for a few decades before being introduced to the market in the United States in 2012 and 2013 called a highly cohesive gel implant or “gummy bear” implant. “Cohesive” is a relative term, referring to the viscosity (firmness) of the silicone gel. The silicone material in these new implants is tightly cross-linked to reduce the amount of silicone gel that escapes into the tissues if the shell ruptures. In fact, you can slice it like a piece of pie without having silicone ooze out (many women have seen this advertised image). These implants are called “form stable” because they are firm enough to maintain their form when in the body, rather than settling into a shape influenced by gravity. But there is a flip-side for this form preservation— these implants do not feel as soft as the original silicone gel-filled implants. The whole point of using silicone is because of its softness, and a jiggle is a desirable quality. They are also much pricier than the usual round silicone gel implants. One popular gummy bear implant, the Biocell Style 410 made by Allergan, caused some undesirable complications, such as double capsules, seromas, malrotation, and pain. More importantly, such “macrotextured” implants are linked to a rare form of lymphoma, Breast Implant-Associated Anaplastic Large-Cell Lymphoma (BIA-ALCL). This implant was removed from the market in July 2019.
Are Shaped Implants Better?
Shaped implants tend to be firmer and are textured in an effort to avoid rotation. They provide greater lower pole projection and less upper pole projection in an effort to simulate a natural (but not necessarily ideal) breast shape. However there are disadvantages to more firmness. Texturing (particularly Biocell implants) may be linked to double capsules, seromas (fluid collections) and even a rare form of cancer, BIA-ALCL. A shaped implant may also rotate and require repositioning. The whole concept of providing more lower pole fullness may be wrong because surveyed women prefer an idealized breast emphasizing fullness of the upper poles (which is why women wear bras). A randomized study found that shaped implants (which are textured in an effort to avoid rotation) really do not provide a superior aesthetic result as once was thought. Today the vast majority of plastic surgeons are inserting smooth, round implants.
Should Old Silicone Gel-Filled Implants Be Removed?
Should silicone gel implants come out if they’ve been in for a long time? It depends. If the patient is happy with the appearance and softness of her breasts (and thousands of women are), she may leave them alone, even if there is a good chance one or both have ruptured. There is a greater likelihood of rupture if they have been in over 10 years. But it’s hard to make a compelling case to remove implants if the breasts are soft, the patient is happy with her appearance, and she is free of any local symptoms, such as capsular contracture.
However, if she is concerned about a change in shape or size, discomfort, or if she is having other cosmetic surgery at the same time anyway, particularly on the breasts, she may decide to have the old implants removed and replaced. Almost any time I reoperate on the breasts, I remove old silicone gel implants, whether ruptured or not, and replace them. This also renews the warranty for silicone gel implants.
Often, women with old (earlier generation) silicone gel implants have varying degrees of capsular contracture. They have gotten used to the excessive firmness of their breasts, even though this can be a problem for them in such social situations as hugging. They may find that they avoid hugging because of their unnaturally firm breasts. They don’t want to advertise the fact that they have had a breast augmentation. This may even make them seem aloof among friends. The problem is not trivial.
An alternative is to remove implants and not replace them, but this is usually not a good option because the breast tissue and skin has been stretched and thinned out for years. She has gotten used to her breasts and will not like the empty, saggy look of her breasts without implants. So I remove the old implants and replace them or remove the old implants and perform a breast lift to take care of the extra slack breast tissue simultaneously. However, a breast lift procedure cannot duplicate the upper pole fullness provided by breast implants. Because this fullness is desirable in women of all ages, I commonly use implants at the time of a breast lift.
Saline Breast Implants
Saline-filled implants have been available almost as long as silicone gel implants. These implants consist of an envelope made of hard silicone (not the soft silicone gel that can ooze into tissues), a self-sealing valve, and are filled with saline—which is simply salt water.
I counsel patients that breast implants are not perfect. They do not feel exactly like breast tissue, which is pliable and easy to squish between the fingers. And saline implants are not quite as soft and squishy as silicone gel implants (although the difference when they are in the body is less obvious).
Someday there may be a more ideal filler material that will provide a truer breast feel, but there are no filler materials presently available with this quality today. Fortunately, for most women this difference in feel is minimal, particularly if the implants are below the muscle and they have some breast tissue of their own over their implants to make them feel softer.
Saline Implants and the Disadvantage of Wrinkling
Even with appropriate maximum filling of implants, wrinkles can be a problem. But we don’t want to inflate the implant too much because of excessive firmness that this would cause. The volumes listed for patients in this section represent the final fill volumes, in all cases close to or at the maximum fill volume of the implants. It would be nice if the envelope were elastic enough to accommodate a wide range of sizes without getting too tight, or forming wrinkles, but the manufacturer needs to balance elasticity with durability. We don’t want nice stretchy implants that leak. Unfortunately, we do not have a perfect implant.
Smooth vs. Textured Implants
The textured implant has a rough surface as opposed to a smooth implant, which has a smooth surface. The theory was that this type of surface would help to prevent the capsule that the body forms around the implant from getting excessively tight, making the breast feel overly firm—the notorious capsular contracture that has long bedeviled plastic surgeons. Does texturing work? There appears to be no difference in the incidence of capsular contracture between smooth and textured implants when the implants are placed below the muscle. So texturing is probably more of a theoretical benefit than a practical one.
Although lightly textured implants are still available (not the macrotextured Allergan Biocell type), few surgeons implant them in the U.S. because it is not clear that the texturing truly represents an advantage and there is a definite link between texturing and BIA-ALCL, even if it is reduced with less aggressive texturing.
A textured surface adheres to the surrounding tissue, in contrast to a smooth implant, which can rotate freely in its pocket, never attaching to the surrounding capsule. The ability of textured implants to adhere to surrounding tissue is used to help anchor contoured implants, so they stay in position and maintain their correct orientation (and an ultrasound study shows that many implants malrotate regardless). Of course, orientation does not matter for round implants, which look the same if they spin.
“Teardrop” Shaped Implants
Sometimes, patients request a contoured or tear drop style implant. They may have done some research and concluded that this will give the most natural look. Contoured (same as “shaped”) implants were popular in the early 1990s and the idea of a less rounded, more natural shape had obvious appeal. However, with experience, plastic surgeons learned that the majority of women do just as well with round implants. Round implants push forward on patients’ natural breast tissue, so they maintain naturally-contoured breasts. In fact, contoured implants may produce less pleasing breast shapes, too vertical with one type and too wide horizontally with another.
At a national plastic surgery meeting in 2014, plastic surgeons in the audience were polled to see if they could tell which patients had shaped implants and which had round. The audience was wrong 55% of the time! A recent randomized study found no aesthetic advantage for shaped implants over round implants.
Implant Profile
The implant profile is a measure of how much the implant projects for a given base diameter. Women desire increased projection and upper pole fullness, so low-profile implants are rarely selected by plastic surgeons. Most of the implants presented in this website are of the moderate-plus profile style. High profile implants are used in women with narrow chests, wanting D-cup sizes, in whom a wide base diameter may be too much for their narrow chest to accommodate (too much “side boob”). And some women simply request high profile implants.
How Long Do Implants Last?
This question is virtually synonymous with “Will I need to have my breast implants replaced?” Certainly, today’s implants are more durable than thinner-walled implants used in the past. But they cannot be regarded as lifetime devices.
Many women who see me in consultation believe that implants last 10 years and then they need to be replaced. This is actually not true. Probably the 10 years figure comes from the length of the warranty. In my own experience, > 90% of women will not need their implants replaced within 10 years. They may last 15 or 20 years, or even more.

*Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166.
Recovery
Immediately after surgery, the local anesthetic is working, so that there is usually minimal discomfort on awakening. The breasts may feel numb or tight from stretching the tissues to accommodate the implants. A sports bra (which fastens in front, making it easy to take off and put back on) is already on. Usually patients wake up quickly after surgery, and are able to go home within an hour. Medication is administered during surgery to prevent nausea, but some women are still be nauseous after surgery, especially in the first 24 hours. Painkillers are needed regularly during the first few days, but then can be tapered and taken only at night. Patients take the prescription painkillers for 5 days, on average. Tylenol may be used as an alternative during the day, but patients should take either the prescribed painkiller or Tylenol, but not both simultaneously to avoid too much acetaminophen (Vicodin and Norco contain acetaminophen too).
I see patients in follow-up the day after surgery. The small dressings under each breast are removed. A semi-transparent adhesive tape (“Steri-Strips”) remains in place over the wound. A folded gauze is placed over the incision to protect it from pressure. The bra is then reapplied.
At home, a bra is used both during the day and night for a minimum of 2 weeks, although most patients wear the bra day and night for a month. After the dressings are removed on the day after surgery, women may take a bath and shower. It is okay to get the breasts wet. The small tapes on the incisions usually stay on and there is no need to worry if they come off in the shower. If they come off, it’s okay just to leave them off.
Sometimes patients notice a sound like “sloshing” after surgery. This is caused by a small amount of air in the pocket surrounding the implant. This air gradually dissolves into the tissues and the sloshing goes away on its own.
Should I Massage My Breasts?
In the past, patients have been instructed to massage their breasts in an effort to reduce the risk of capsular contracture, although such a benefit has never been demonstrated scientifically. Most plastic surgeons, including myself, do not recommend massage. I believe it can do more harm than good.
Swelling and Bruising
After surgery, the breasts are swollen and bruised. Almost always, one breast swells and bruises more than the other. This is normal. There may be very little bruising, or the bruising may cover a large area, sometimes all the way down the abdomen. This appearance can be quite dramatic, but normal and nothing to worry about. The bruising results from blood that trickles down under the skin, pulled by gravity. As this blood is absorbed by the body, the bruising goes away, usually within 1 month.
The swelling gradually goes down over a period of about 1 month, too. In patients who had loose skin before the procedure, usually from pregnancy, the early appearance is often very natural. In patients who have not undergone the stretching process from pregnancy, the breasts may feel very tight after surgery. Gradually the skin stretches to accommodate the implants. As the skin stretches, the implants gradually settle. The appearance improves as the breasts become more pendulous, adopting a more natural appearance. The cleavage gradually appears. Excessive, painful swelling and bruising, much more on one side than the other, needs to be brought immediately to the attention of the plastic surgeon, because this may signal the development of a hematoma. When it occurs, this complication almost always happens within the first 12 or 24 hours after surgery.
Postsurgical Apprehension
Patients worry that others will notice right away that they have had a breast augmentation. They are often surprised that friends do not usually notice, particularly in loose-fitting clothing, so that this is not as much of a problem as they expected.
Women may worry at first that their breasts are “huge” and “too high”—this reaction is expected. The envelope gradually expands to accept the implants and the swelling goes down. After 1 month, the swelling is gone and the implants may still be a little high, although this is not objectionable for most patients who enjoy their newfound perkiness. After several months to a year, the breasts tend to settle into a more natural position.
Numbness/ Painful Sensations
In making the incision, small, superficial nerves in the skin are cut and, in making the pocket for the implant, larger nerves are stretched. A major sensory nerve to the nipple comes from the side of the rib cage (lateral branch of the fourth lateral intercostal nerve). This nerve is stretched during surgery. In making the pocket, I use my fingers to tease the muscle off the chest wall on the sides. This way I can feel the deep nerve branches and preserve them.
The skin is numb right after surgery. For the first several hours, this numbness is due to the long-acting local anesthetic (bupivacaine) that was injected into the tissue in the operating room. Later, the sensory nerves send varied signals, such as pain, burning, or extra-sensitivity. These sensations can sometimes be distressing and seem to suggest that something is wrong. It is not uncommon for me to receive anxious calls from patients about these unusual sensations. Gradually, over the course of about 2 months, these uncomfortable feelings subside as the nerves recover.
Patients may feel muscle spasms, usually around the sides of the breasts. These are also a normal and temporary consequence of a submuscular breast augmentation. Patients are often surprised that these feelings are more pronounced on one side than the other (thinking quite reasonably that the discomfort would be similar on both sides), but in fact there is usually more discomfort on one side than the other, just as there may be more bruising and swelling on one side than the other.
Temporary Loss of Feeling
Patients may notice a band they can feel under the skin at the crease under the breast (“inframammary fold”). This is due to some tension from the wound closure and some early normal scarring of the tissues under the skin. It gradually softens.
All women have loss of some feeling in their skin after surgery. This feeling gradually returns as the little nerve branches in the skin regenerate. There may be some loss of feeling in the nipple due to stretching of the nerves, but this is usually temporary and gradually returns. In our survey, only 2% of patients had persistent (2 years or more) loss of sensation of one or both nipples after breast augmentation (Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166). The number of patients reporting loss of nipple erectility was similarly low in our study. There may be loss of the normal reactivity of the nipple to stimulation, but this also gradually returns in almost all women. Sometimes one nipple will “wake up” before the other. Typically, if nipple numbness is experienced (39% of women report at least temporary numbness), normal feeling returns within a few months (2½ months on average).
The Bra
After surgery, the body gradually forms a capsule around the implant. A benefit of wearing the bra after surgery is that it helps hold the implants in their proper position while the capsule forms during the first couple of weeks after surgery. A sports bra that comes together in front may be used. This is more comfortable than a regular bra because it is difficult at first for most women to reach around their back during the first week after surgery. The bra fits snugly, helping to hold the breasts together, so that the capsules form in the right location, allowing a pleasing cleavage. The cleavage is usually not apparent right away, but as the swelling goes down and the tissues loosen, the cleavage becomes more defined. The bra should not fit too tightly. It should feel comfortable and patients should forget they have it on. The straps should not dig in to the skin. Patients report that they are more comfortable wearing a bra than not wearing one. The pull of gravity can be uncomfortable at first. Even a car ride can be uncomfortable. The bra provides protection and support.
Light Activity
Patients can walk right away after surgery and perform light tasks. However, certain arm movements that involve the pectoral muscles, such as pushing up from bed, fixing hair, or pulling open a heavy door, are going to be sore. Heavy housework, or lifting groceries is to be avoided. Patients can certainly lift a small child if they need to—they are not going to damage anything—but they are likely to be sore and may swell more. Women should have someone around to help with small children for the first 3 or 4 days after surgery.
Pain Control
Painkillers are needed regularly during the first few days, but then can be tapered and taken only at night. Patients take the prescription painkillers for 5 days, on average. Tylenol may be used as an alternative during the day, but patients should take either the prescribed painkiller or Tylenol, but not both simultaneously to avoid too much acetaminophen (Vicodin and Norco contain acetaminophen too). Many patients wish to limit their consumption of narcotic painkillers.
Ibuprofen can be substituted in many patients after a few days.
It is important not to exceed the maximum daily dose of either acetaminophen (4000 mg) or ibuprofen (3200 mg).
Resuming Activities
Patients may drive when they are no longer taking prescription painkillers during the day. Our survey found that the average patient starts driving again 5 days after surgery. Most patients who work at office jobs are able to return to work in 1 week. However, those whose jobs are more physical (such as waitresses, nurses, and flight attendants) may require 2 weeks. Patients whose work is very physical (assembly line worker, parcel courier, massage therapist) will need 3 weeks to recover. It is important to remember that the breasts will be sore for at least a month after surgery.
Patients may start cardiovascular workouts 2 weeks after surgery—walking at a fast pace on a treadmill, for example. Between 2 and 4 weeks, activity may be increased. Aerobics may be started at 3 weeks. Unrestricted exercise is permitted at 4 weeks. Of course, these are simply guidelines. Every patient is different in their recovery times, and in their ability to withstand discomfort. If the breasts are hurting, or become swollen after exercise, it’s too early. Patients report being “back to normal” at 3½ weeks, on average.
Asymmetry
Many women are unaware of subtle existing differences in the shape and size of their breasts. Plastic surgeons point out these differences because patients tend to look more critically at their breasts after surgery. It is common for one breast to be larger than the other. One implant may be inflated slightly more than the other (when using saline-filled implants) to compensate for small differences (<30 cc) in volume. If the asymmetry is greater, exceeding the fill range of a specific implant size, different implant sizes may be used.
How Do Breast Implants Feel?
Breast implants are certainly not a perfect substitute for breast tissue. They do not feel like breast tissue. They are firmer, and can be felt, especially laterally, on the underside of the breast, where they are not covered by the pectoralis muscle.
Sometimes breast implants develop ripples (also called wrinkles) that can be felt or even seen. For this reason, additional inflation of the implant, called overfilling or, more accurately “maximum filling” is done routinely by plastic surgeons to help prevent this problem. Why do ripples happen in the first place? In an effort to make more durable implants that do not rupture, the manufacturers have used thicker envelopes, which can form ripples, even when the implant is maximally filled. Furthermore, in thin women, it is sometimes possible to feel the bump at the site of the valve (these are present in saline implants, not silicone gel implants), even when the implant is under the muscle.
Better Proportions
Breasts naturally fall to the side because of the curvature of the chest wall. Women who have never had large breasts may be surprised that they can now feel the sides of their breasts touching their upper arms. This is normal, and women get used to this new sensation. In fact, it would be abnormal for women not to feel their breasts on the sides. Breasts do not naturally project straight ahead like torpedoes. When a woman lies down, in a bikini on a beach for example, the breasts should naturally settle slightly to the sides. This fullness on the sides helps give a pleasing feminine contour. It balances the curve of the hips. The upper body now complements the lower body.
Cleavage
Part of the purpose of a breast augmentation is to reduce reliance on external devices such as a Wonder-Bra or bra inserts. No woman likes wearing bra inserts; it is much better to achieve cleavage with a regular bra. Most women with larger breasts, whether natural or augmented, will still need a bra for cleavage, because breasts normally settle to the side due to the curved contour of the rib cage.
The area between the breasts is a test of the quality of a breast augmentation. Everyone finds the “half grapefruit stuck to the chest” appearance unnatural. The edges of the implant can be seen, producing an unnatural demarcation around the circumference of the implant. It almost looks as if the breast could be moved around on the chest like a pool ball on a pool table! This non-ideal result is found even in well-known models and actresses. If the implants are placed above the muscle, there will be a flat-bottomed valley between the breasts which rise up like bookends on either side. Consequently, most plastic surgeons place breast implants under the muscle, to add tissue and to help obscure the implant margins. If the implants are simply placed under the muscle without releasing the muscle, particularly in a thin patient, the distance between the implants will be too great, and it will be difficult to produce a cleavage.
So how do we get a nice cleavage and still have the implant under the muscle? By carefully releasing the pectoral muscle from its attachment to the lower part of the breastbone (sternum). This maneuver allows the pockets that accept the implants to be situated close to each other in the middle, separated by a small valley—a V instead of a U. The right amount of muscle release is the key to an ideal result: Not enough release and the valley is too wide; too much and the breasts unnaturally abut each other in the middle, or some of the cleavage is filled in, a complication called “synmastia”.
Will I Sag More Later on If I Have Implants?
It’s a good question, but unfortunately one without a good answer because no study has evaluated sagging in women with and without implants.
We know that sagging is related to heredity, age, weight of the breasts, pregnancy and substantial weight loss. Among these factors, breast implants affects only one—the weight of the breasts. With additional weight, it would seem reasonable that augmented breasts would sag more with time and gravity. It makes sense that larger implants would cause more sagging because they are heavier. But this is just working from first principles. The trade-off of possibly more sagging needs to be balanced against the “here and now” benefits of a breast augmentation. A breast lift may be performed years from now, and the implants may or may not make this more likely.
Implants do settle with time. This fact is taken into consideration by experienced surgeons in creating the pockets for the implants at the time of surgery. I tell patients to expect the implants to look too big and too high right after surgery. Nevertheless a common reaction after surgery is: “Doctor, they are too big and too high!” And my response is: “Give them a few months to settle, and they will be just right.”
Breast Implants and Pregnancy
Fortunately, saline-filled implants have no known harmful effect on fertility or breast milk. Saline-filled implants do not hold any silicone gel that may ooze into the surrounding tissue, and saline solution is harmless. Reports indicate that even silicone gel implants are safe because of the extremely minute quantities of silicone that gets into the breast milk. Evidently, cow’s milk contains more silicone than human breast milk from women who have silicone gel implants! Breast tissue swells as it engorges with breast milk, regardless of whether an implant is located close by, just behind the pectoral muscle. When the breast tissue shrinks after pregnancy and the completion of breast feeding, the breasts will get smaller, but this reduction will be limited by the implants, so that apparent breast shrinkage will be limited. This is an advantage for women who had implants inserted before their pregnancy.
Of course, waiting to have the surgery until after child-bearing is an option, but this is not medically necessary. Women can enjoy the benefits of their augmentation before, during, and after their child-bearing years.
Breast Implants and Mammograms
Even though they are filled with salt water (“saline”), breast implants still interfere with mammograms by casting a shadow. Nevertheless, it is still possible to perform mammograms with special views. Recommendations for self-examination and mammograms remain the same after augmentation as they did before. If you are due for a mammogram, it is best to have this done before your breast augmentation, so that normal scar tissue after surgery is not a source of confusion to the radiologist.
Reoperation
There are certain outcomes that need to be regarded as unavoidable and acceptable, at least with saline-filled implants available today. For example, slight asymmetry or wrinkling that you can feel is regarded as normal. On the other hand, visible rippling or excessive hardness is unacceptable. If a patient has a result which is almost ideal (for example, one breast looks very slightly higher than the other), it is usually better to accept this imperfection rather than to reoperate. An old adage applies, “Great is the enemy of good.” In other words, the risk and unpredictability of additional surgery may outweigh the marginal improvement that may be possible if everything goes just right and the body heals just the way you want.
Surgeons differ widely as to what level of result is acceptable and what deserves a “redo.” Some surgeons even consider reoperation rates an acknowledgment of failure and tout low reoperation rates as a sign of proficiency. However, all surgeons have suboptimal results and the perfectionistic surgeon will want to do the best he or she can for the patient and this may mean a reoperation—or the prudence of not reoperating.
Indeed, reoperations or touch-ups are a part of cosmetic surgery. They should not be regarded as failures. Patients are generally pleased, but simply need some additional “fine tuning.” Knowing when to reoperate and when not to reoperate comes with experience, and it can be a challenge, even for experienced surgeons. Part of the decision involves the patient’s attitude and expectations. If the patient expects perfection, or has an exaggerated importance placed on relatively small physical details (i.e. “Body Dysmorphic Syndrome”), additional surgery may be unwise.
Wrinkling
This is the most common complication of breast implants. Usually it is possible to feel, but not see the rippling in the envelope. This is especially true on the underside of the breast, where the implant is not covered by muscle. But sometimes the rippling is apparent, especially in thin women.
Nipple Numbness
It is important to preserve the intercostal sensory nerve branches by using gentle finger dissection of the lateral pocket during surgery. Almost 40% of patients experience some degree of nipple numbness after surgery. In my experience, very few patients (2.3 percent) have persistent loss of feeling in one or both nipples after breast augmentation. Almost all patients (98.5 percent) would have the surgery again, despite any experience of nipple numbness.
Capsular Contracture
The body always forms a capsule around implants. This is normal and desirable. However, sometimes the capsule becomes firm and tight. This is called a capsular contracture. Why does this happen? We do not know. Perhaps it is part of the body’s response to the implant. Some researchers think a “subclinical” (no clinical signs) infection might be responsible.
What causes the capsule to tighten? Tiny cells in the capsule lining perform a microscopic “tug-of-war” on the collagen fibers. There is nothing wrong with the implant. It is sitting innocently in the pocket while it is being squeezed by the lining that encases it. It is compressed into a more spherical shape. This shape is not a coincidence—a sphere is the smallest surface area-to-volume relationship. Not only do we not know why this complication occurs in women, we also do not understand why it usually happens on one side and not the other. You would think the body would react the same on both sides.
As a result of this tightening, the implant is pushed in the direction of least resistance, usually up. Treatment calls for a return to surgery to have the capsule released, called an “open capsulotomy.” The implant is repositioned at a lower level.
Open Capsulotomy
Fortunately, an open capsulotomy, done under a brief intravenous sedation with the patient asleep, is not painful and patients can get back to most of their usual activities right away, even returning to work the next day, or after a weekend. The procedure is minimally painful because the amount of dissection is limited. The surgeon simply cuts the capsule lining on the inside. The pocket has already been developed, so there is no dissection lifting the muscle off the chest wall.
Once the capsule is released with an open capsulotomy, the pressure on the implant is immediately relieved and the breast softens. It is possible for a contracture to reoccur, but fortunately, this is unlikely. The capsule does reform, but it usually does not again tighten down on the implant sufficiently to cause a capsular contracture, although I have had occasional patients who required a second capsulotomy. In these patients, there is more commonly a history of ruptured silicone gel implants. Even though we do not know why capsular contractures occur in some patients and why it usually does not recur, in our ignorance perhaps we should be thankful that this complication does not always happen with implants.

Does the Capsule Need To Be Removed?
A common belief is that infection is responsible for capsular contracture. However, there are problems with this theory, including the fact that this complication can sometimes occur years after breast augmentation and only on one side. Many surgeons recommend removing the entire capsule (called a capsulectomy). The conceptual basis for this procedure is unclear because even a capsulectomy cannot make the breast pocket sterile (breast tissue normally is occupied by harmless “commensal bacteria”). A capsulectomy can be a traumatic procedure, increasing risks such as bleeding, nerve injury, pneumothorax, and skin loss. The surgery takes longer. It is also more painful for patients, difficult to recover from, and expensive. The alternative is simply to leave the original capsule in place, provided there is no evidence at surgery of an abnormality. This has been my practice for over 2 decades. The recurrence rate is 22.7%, which compares favorably to capsulectomy (which can be as high as 53%). The recurrence rate is even lower (13.6%) for intact (nonruptured) breast implants. Patients have very little downtime, the expense is minimal, and the breasts are minimally traumatized. Although some women will require a second release, it is very unusual to need a third.
Swanson E. Open capsulotomy: An effective but overlooked treatment for capsular contracture after breast augmentation. Plast Reconstr Surg Glob Open 2016;4:e1096.
Acellular Dermal Matrix (ADM)
Recently, some surgeons have proposed using mesh taken from cadavers (Alloderm) or pigs (Strattice), manufactured by Allergan (now Abbvie, Chicago, Ill.), in an effort to reduce the risk of a recurrent capsular contracture. Some plastic surgeons have even used this biological material in patients at their original breast augmentation when they believe the patient is at high risk of developing a capsular contracture. Although this skin stripped off cadavers or pigs is processed to make it aseptic, there is still a small risk of disease transmission. The risk of such complications as seromas and infections is increased. Also, it is not clear that it works. Many investigators have financial conflicts with the manufacturer. The material is not cheap, typically over $5000. This material is not yet approved by the FDA for breast surgery (it is approved for treatment of hernias). The bottom-line question for plastic surgeons who promote it: Would you use it in a family member? Much better to simply perform an open capsulotomy at minimal risk. The risk/benefit ratio is simply not favorable for ADM.
- Swanson E. Open capsulotomy for capsular contracture after breast augmentation: An alternative treatment algorithm. Plast Reconstr Surg. Slated for acceptance October, 2020.
- Swanson E. Concerns regarding the use of acellular dermal matrix at the time of primary breast augmentation. Ann Plast Surg. 2021:86:1–2.
Breast Implant-Associated Anaplastic Large-Cell Lymphoma (BIA-ALCL).
In 2015, a landmark paper by Brody and colleagues identified a link between textured breast implants and a rare form of lymphoma called BIA-ALCL. The risk was thought to be very low, on the order of perhaps 1 patient in 500,000. However, over time, it has become apparent that the risk is much higher. Dr. Cordeiro, a plastic surgeon performing reconstructive breast surgery in New York City, found that the risk over 20 years in a woman implanted with Biocell textured breast implants is about 1:100!
The reader might ask, why did plastic surgeons use textured breast implants in the first place? The reason was twofold. One reason was to help reduce the risk of capsular contracture. It was thought that the little ridges on the implant would help to do this. The other reason was so that the implant could adhere to the local tissues, which is important if the surgeon uses a shaped implant so it does not rotate and cause asymmetry. Later we learned that texturing the surface probably does not really reduce the capsular contracture rate and shaped implants don’t actually look better than round ones.
In 2019 the FDA issued a ban on macrotextured (Biocell) implants. Smooth implants are still available. There are some women who have developed BIA-ALCL after having smooth implants, but it is not 100% clear that they did not at some point have textured implants. So the link to textured implants is very strong. Implants with a lighter degree of surface texturing are still available, but many surgeons, particularly in the U.S., do not use them because there is probably no advantage in a light texturing anyway. Bottom line: today it is best to use smooth, round breast implants.
- Swanson E. Textured breast implants, anaplastic large-cell lymphoma, and conflict of interest. Plast Reconstr Surg. 2017;139:558e–559e.
- Swanson E. A 1-point plan to eliminate Breast Implant-Associated Anaplastic Large-Cell Lymphoma (BIA-ALCL). Ann Plast Surg. 2018;80:565–466.
- Swanson E. The textured breast implant crisis: A call for action. Ann Plast Surg. 2019;82:593–594.
- Swanson E. The Food and Drug Administration bans textured breast implants: Lessons for plastic surgeons. Ann Plast Surg. 2020;84:343–345.
Breast Implant Illness
Many women with breast implants have become ill. This has happened to women with smooth implants, textured implants, saline implants, and silicone gel implants. The ailments include such problems as memory loss, joint pains, fatigue, rashes, and headaches. In fact, the list is much longer, including about 80 different symptoms. Exactly how breast implants cause such problems remains unknown. The evidence is largely circumstantial. No randomized studies have been conducted (and these would not be possible in a free society). As women age, they are more likely to develop such problems even without breast implants.
So what does the woman who has developed new symptoms do? The first step is obviously to investigate and treat the problem. Whether to remove her breast implants is a thorny question indeed. Some women who have their implants removed report a resolution of their health problems, but others do not. I have had patients remove their breast implants, experience no change in symptoms, and return to have breast implants reinserted.
Should the Breast Capsule Be Removed?
Many plastic surgeons recommend that not only the breast implants be removed in the setting of Breast Implant Illness, but the capsule as well. In fact, there is even a website called “enblocsurgeons.com” where patients can look up an “en bloc” surgeon, who is committed to removing every piece of the capsule along with the implant. Prices are >$10,000.
If a capsulectomy were easy and harmless, why not? Well, it is not easy and harmless. It is often a difficult dissection with a high complication rate. It can leave the breasts looking scarred and deformed, much worse that they appeared before the breast implants were inserted. Plus, there is no scientific basis for capsule removal in a woman who has normal breast capsules. An en bloc capsulectomy is unnecessarily aggressive.
A much better option for the woman who has textured implants but no sign of capsular disease or BIA-ALCL, is simply to have her textured implants exchanged for new smooth implants. This is a short, inexpensive, and safe procedure.
Today, there is no reason for women to have textured implants. Both cosmetic augmentation and reconstruction may be performed with smooth implants, avoiding the risk of BIA-ALCL.
- Swanson E. Breast implant illness, biofilm, and the role of capsulectomy. Plast Reconstr Surg Glob Open 2020;8:e2999.
- Swanson E. Evaluating the necessity of capsulectomy in cases of textured breast implant replacement. Ann Plast Surg. 2020;85:691–698.
- Swanson E. The case for breast implant removal or replacement without capsulectomy. Aesthetic Plast Surg. Accepted November 2020.
Implant Leakage
Implants do not typically leak because of physical or sexual activity and I counsel my patients that they do not need to treat their breasts any more carefully after healing from breast augmentation than before surgery. If an implant leaks, it does so without provocation. Indeed, the cause is usually a leak at a fold in the envelope. These problems are related to the implant itself and cannot be controlled by the patient. Typically, such a patient calls my office and reports that one side just seemed to deflate and she wasn’t doing anything strenuous when it happened. The procedure to replace a deflated implant is very short, and there is almost no postoperative pain, because there has been very little new dissection at surgery. The pocket is already developed and it’s just a matter of putting in a new implant through the same old incision. Patients are usually back to work in a few days.
Deep Venous Thrombosis
Blood clots may rarely develop in the leg veins after breast augmentation. To reduce risk, patients are not given muscle relaxants during surgery. Routine screening with ultrasound is used to allow early detection and treatment of any deep venous thromboses that develop after surgery.
- Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96.
Hematoma
Bleeding is a possible complication after most types of surgery and breast augmentation is no exception. This complication is on the minds of all plastic surgeons and nurses in the period immediately after surgery. Detection requires vigilance on the part of the patient and surgeon. Hematomas typically occur within the first 24 hours after surgery and most of these occur within the first 12 hours. If one breast swells dramatically more than the other, filling the upper pole below the collarbone, and if there is much more pain on one side than the other, this probably indicates a hematoma—postoperative bleeding that requires immediate attention. Usually patients hold their arm on the affected side close to their body and cannot reach out without pain. A clot may have come loose from a small artery that was divided when the pocket was made at surgery. The wound must be reopened and the blood clot removed. Any bleeding is controlled with cautery.
Provided the hematoma is detected early, and treated, the outcome is excellent. One reason I see patients the day after breast augmentation is to make sure they don’t have a hematoma. Also, I insist that out-of-town patients stay in the area at least 24 hours so they don’t have far to come if they do develop this complication.
Implant Malposition
Sometimes one implant settles more than the other. An implant may be pushed up by a capsular contracture. The treatment is the same—repositioning the implant.
Infection
Infection is a risk in all operations. Patients are given antibiotics as a preventative measure. Patients may develop infections that will necessitate removal of the implants to eradicate the infection. New implants may then be inserted once the infection is clear. Fortunately, this is a rare occurrence.
Hypertrophic Scars
Excessively wide or thick (“hypertrophic”) scars may develop at the sites of the breast incisions if a patient is predisposed to these unfavorable scars. Fortunately, the inframammary scars are in an inconspicuous location.
It is okay to wear a sports bra instead of the garment provided at the time of surgery. Because of the pressure from the wire, avoid underwire bras for 1 month.
Avoid vigorous exercise for at least 2 weeks after surgery. During the first 2 weeks the implant is settling into location and should not be subjected to movement. Vigorous activity also increases swelling, and should be avoided.
Avoid heavy lifting (> 20 pounds) during the first 2 weeks. Women with small children need to avoid lifting during this period and will therefore need assistance for 3 or 4 days. Do not perform heavy housework, mow the lawn, or lift heavy bags of groceries.
You may resume exercise gradually, performing light cardiovascular exercises 2 weeks after surgery, such as walking on a treadmill. Full aerobic exercising may be resumed 1 month after surgery without restriction. Keep in mind that everyone heals at a different pace. Your body will tell you (pain, increased swelling) when you’re overdoing it. If you work out and feel fine the evening and night afterward, you can gradually increase your workout the next day. Avoid jumping back into your usual routine even if you feel okay while you are doing it. You’ll hurt and swell more later.
A low-grade fever (< 101°F) is normal during the first 48 hours. Report any persistent fever, increasing rather than decreasing pain or swelling, or any drainage from the incision that persists longer than 2 days.
Most patients are able to return to work approximately 1 week after surgery. If you have a more physical job (server, nurse, factory worker), a period of at least 2 weeks will be necessary. Remember that you will still be sore for about 1 month.
Wait until the bruising is gone before using a tanning bed. Protect the incisions under the breasts with Band-Aids. The incisions will heal with a less conspicuous scar if they are protected from UV exposure for at least 1 month.
Q: What incision do you use?
A: Inframammary (actually “supra-inframammary”): The incision is located on the lower part of the breast, just above the crease under the breast. My second choice is periareolar, making use of the natural border around the areola to hide the scar. I rarely use the axillary incision that leaves a scar in the armpit. It is more difficult to dissect the breast pocket precisely using this more remote access.
Q: Over the muscle or under the muscle?
A: Under the muscle. The breast appears more natural, feels more natural, and there is less risk of a capsular contracture.
Q: Do you use contoured (shaped) implants?
A: No. As it turns out, it’s hard to tell any difference between round and contoured implants when they are in the body. Contoured implants are textured and we know that BIA-ALCL is linked to textured implants. Contoured (shaped) implants cause disproportionately greater fullness of the lower poles, and may rotate, causing asymmetry.
Q: Do I have to have my implants changed out in 10 years?
A: This is a common question. No, there is no need to have breast implants replaced in 10 years. If you do not have a deflation, they may last much longer than 10 years. Nevertheless, you should count on having another breast operation at a future date, whether it is in 6 months or 15 years, we do not know. The most common reasons are to change to a different size (usually larger), release a capsular contracture, or to replace a deflated implant. Deflation is associated with saline implants.
Q: Will I lose feeling in my nipples?
A: This problem is related to the surgical technique. By using finger dissection of the pocket laterally, it is possible to avoid injuring the lateral cutaneous branch of the fourth intercostal nerve, which supplies the nipple. Sensation may be decreased after surgery from stretching but almost always returns to normal.
Q: Should I wait until after having children?
A: There is no medical reason to wait.
Q: Can I still breastfeed?
A: Breast augmentation does not interfere with your ability to breast feed. Keep in mind that not all women can successfully breast feed. However, if you’ve successfully breastfed your children before, it is likely that you will still be able to nurse after your augmentation.
Q: Should I have a mammogram first?
A: Recommendations regarding mammograms do change from time to time and it is best to defer to the advice of your primary physician. If you are due for a mammogram, have it done before your breast reduction. You can have mammograms after the breast reduction, but it is best to schedule this at least 6 months after your breast augmentation, unless there is a medical reason (like a lump) to do so earlier.
Q: What is the risk of deflation?
A: About 1–3% over 10 years for saline-filled implants.
Q: Silicone or saline?
A: Both work well. The appearance is very similar and any feel advantage for silicone gel is made less by the overlying tissue. However, if you are very thin and have very little breast tissue, and are concerned about wrinkling, you may consider silicone gel.
Q: How do you know what size to use?
A: The selection of size is more art than science. Although there are measurement systems available, these tend to underestimate implant size. Inserting implants in the bra is not particularly helpful because this does not accurately reflect the change in size that is created by an implant that is placed in the body.
Ideally, the patient achieves the size she wants in one operation. After talking with my patient, examining her, and looking at pictures of other patients with her, I have a good idea what she wants. Many women show me photos on their phone, which is helpful too.
In my practice, almost no one says they are too large at the time of their 1-month follow-up appointment. I do have the occasional patient that wants to be larger. Over a 5-year period, five patients returned for larger sizes. No one returned to have the implants changed to a smaller size. It is often difficult even for patients to know what size they want before surgery. Some patients become more appreciative of their breasts after surgery and less inhibited about a larger size.
Q: When can I return to work?
A: Most patients return to work in a week, but there certainly is a range. Some women get back to work in a few days and others are glad they took a week off. If you have a physical job, 2 to 3 weeks off is better.
Q: Do you use a pain pump?
A: No. Although it sounds like a good idea, “pain pumps” (actually local anesthetic infusion devices) have not worked well in practice. Patients find them cumbersome and pain scores with the pump were not significantly better than patients treated without a pump in a controlled double-blind study.