INTRODUCTION
Problems With Very Large Breasts: Physical and Psychological
Women who have large breasts endure at least as much psychological pain as those with small breasts. Added to this are the common physical symptoms—back, neck, and shoulder discomfort. Physical activities and sports are limited. Usually patients with large breasts have lived with these symptoms for years. Many have had chiropractic care. Patients regard their breasts not as a positive part of their anatomy, but as a negative. Sometimes patients will declare to me, “I want them off!” After surgery, it is common for patients to say, “I wish I had done this earlier.” The quality of life for women with very large breasts is surprisingly bad. One study found that living with excessively large breasts is comparable to the burden of living with moderate angina or a kidney transplant!
Often, women with very large breasts develop poor posture and know this compromises their attractiveness. Some have indentations on their shoulders from their bra straps. They can suffer skin irritation and infections under their breasts (“intertrigo”).
Young women often tell me they have problems participating in sports since their breasts can literally get in the way. In order to jog comfortably, they must wear two sports bras, which is hot and uncomfortable. Large-breasted women have difficulty finding clothing that fits well and bras that give enough support. I had one patient whose breasts were so large she always wore a bra to bed out of fear that one might smother her as she slept!
Happily, we have the tools to help these women. It is hard for me to imagine past generations of women who went their whole lives with this encumbrance, a literal weight on their chests, without the benefit that a 2-hour procedure could make in their lives.
Today, breast reduction surgery aspires to more than just a functional benefit in relief of symptoms. It is also a procedure to improve the appearance of the breasts. For the majority of breast reduction patients (90%), improvement of appearance is part of the reason they are having surgery.
Turning Point: Making a Change With Breast Reduction
Breast reduction is one of the most satisfying procedures for the patient and plastic surgeon alike. I particularly enjoy the procedure both from a technical standpoint because of its demands for finesse and rewards for attention to detail and from the immense satisfaction of patients afterward. The significance is so profound that patients will often think of events in their life in chronological terms before and after their breast reduction. For example, “We went on that cruise 6 months after my breast reduction.” Similar to breast augmentation, a breast reduction brings an immediate smile to patients’ faces. Patients are often happy even in the recovery room waking up after surgery. There is much to be said for immediate gratification.
The breasts are simultaneously tightened and reshaped, so patients also receive the benefit of a breast lift when they undergo a breast reduction. Not only may the breast size be reduced, their appearance may also be improved. Women find they now have a flattering torso that was previously obscured. They look thinner. Friends think they’ve lost weight. They can wear dresses that they could not wear before. They can go braless. They can exercise without the encumbrance of heavy breasts and unwanted attention. A weight has been lifted off their chests, literally and psychologically. This can be a turning point in a woman’s life. Patient satisfaction rate is very high, on the order of 95%. This level of patient satisfaction in plastic surgery is rivaled only by breast augmentation and abdominoplasty.
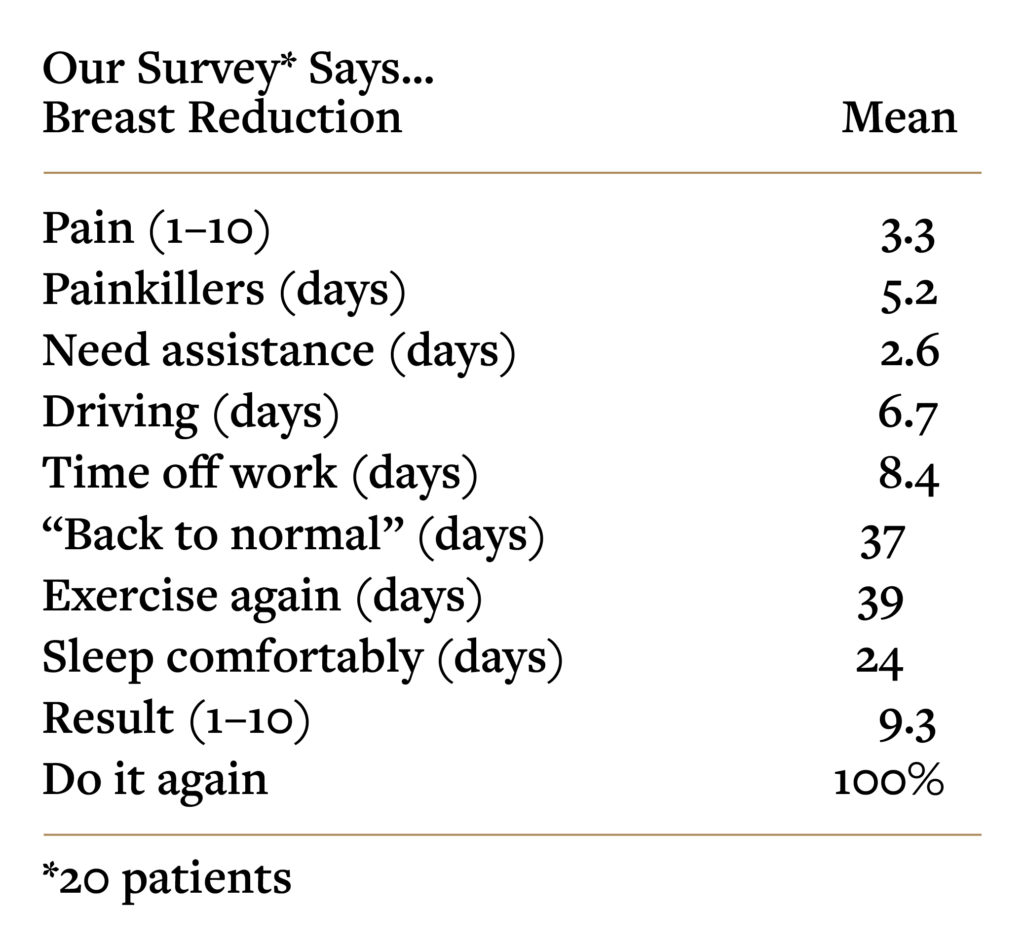
Despite the fact that the surgery takes longer and there are more incisions, a breast reduction is usually less painful than a breast augmentation, because there is no lifting of muscle or stretching of tissues. The average pain score of patients having a breast reduction is 3.3 on a scale of 1–10, compared to 5.9/10 for patients having a breast augmentation.
Age
Older age is not a barrier, and older women often elect to have this surgery because with age their breasts have gotten larger and become more uncomfortable.
It is uncommon to perform this surgery on teenage girls until their breasts are fully developed. Occasionally I make an exception for a teen who has developed very large breasts at puberty and will suffer psychological damage if this problem is left unattended. Too many large-breasted women have related such stories to me of traumatic teenage years to ignore this reality. Breasts may continue to enlarge after a reduction, so young women need to know that another operation may be necessary later on, but the scarring will be no more extensive because the same incision is used for redos.
Insurance Coverage
Because of the physical problems associated with large breasts, which have been well-documented in numerous studies, insurance companies may provide coverage. When a woman comes to see me to discuss this surgery, I take photographs and send a preauthorization request to her insurance company. The insurance company has physician reviewers who make the decision as to whether the procedure is medically necessary.
Insurance companies sometimes deny applications for women who will truly benefit both physically and psychologically from this surgery. There may be a clause excepting breast reduction, or the reviewer may simply turn down the application, judging the breasts not large enough to qualify. Of course, the reviewer’s job is to sort out the cosmetic patient, whose interest is largely her appearance, from the breast reduction patient who has physical complaints due to breast size. This is a judgment call because there is obvious overlap. We now know that women with smaller degrees of breast hypertrophy, even less than 300 grams per side, can be symptomatic (Swanson E. Prospective outcome study of 106 cases of vertical mastopexy, augmentation/mastopexy, and breast reduction. J Plast Reconstr Aesthet Surg. 2013;66:937–949). And, not surprisingly, almost all women are at least partially concerned with the appearance of their breasts.
Scarring
A woman considering this surgery must know that she will have visible scars on her breasts, identical to the scars left by a breast lift. The skin incisions are the same. In a breast reduction more excess breast tissue is removed. A breast lift typically removes less breast tissue. The number of grams of breast tissue separating the procedures is arbitrary. Some insurance companies use an estimated resection of 500 grams per side as a benchmark, which is too high. I define a breast reduction as removal of at least 300 grams from at least one breast.
Most women consider the scars a small price to pay for the benefits, which in the case of a breast reduction go beyond improved shape and position to also include physical relief. The cost/benefit ratio heavily favors the procedure, so much so that women with suboptimal scars are still almost always glad they had it done. All of the breast reduction patients in our survey reported they would “do it again.”
Breastfeeding
Ironically, many women with large breasts find they cannot breastfeed successfully even before breast reduction surgery. Modern techniques that preserve the nipple on a pedicle allow for the possibility of lactation because breast tissue is preserved in continuity with the underlying tissue. The proportion of women able to breastfeed after breast reduction surgery is in the range of 62–72% according to one study. This range is similar to the rate for women with large breasts who do not have surgery. But any woman having a breast reduction needs to accept the possibility that she may not be able to breastfeed afterward.
Nipple Grafting Is Obsolete
Free nipple grafting is an old technique that involves removal of the nipple as a graft during surgery and replacement as a graft. This operation divides the attachments of the small ducts leading into the nipple and the nerves. Patients who have this procedure cannot breastfeed and lose feeling in their nipples. That is why it is done very infrequently today. In fact, I have never had to resort to this procedure in practice. Now that we have learned how to elevate the breast tissues using the vertical technique and minimize nipple transposition, nipple grafting has become unnecessary.
Smoking
Like a breast lift, breast reduction undermines skin flaps and partially divides the circulation. Nicotine further reduces circulation by causing the small blood vessels to clamp down, choking off the flow of oxygen and nutrients to the skin edges. This means the skin furthest out on the skin flap may not survive. This leads to skin loss, usually along the edges of the incisions. A crust forms and gradually the skin heals in on its own, but the wound takes longer to heal and the scar is wider than it would have been. Because the vertical technique avoids skin undermining, this procedure may be done safely on smokers, but patients are still informed of the risks and asked to stop smoking at least temporarily 2 weeks before and 2 weeks after surgery, to allow a margin of safety.
Breast Reduction Over 50
Women who have put off this procedure for years invariably wonder why they did not do it when they were younger. There is no specific age limit, and women of all ages can enjoy an improved quality of life afterward. Recovery is easy.
Suboptimal Scars
One method of doing a breast reduction avoids a vertical scar. There is just a circular scar around the areola and a horizontal scar in the inframammary fold. This sounds like an attractive option. However, in avoiding a vertical scar, there is no tightening of the lower breast pole from side to side, leaving an unattractive boxy appearance to the breast. There is still a long horizontal scar, which is the scar patients find objectionable. From either a scar or shape perspective, this approach is suboptimal and it has not been adopted by many plastic surgeons in practice.
PHOTOS OF PATIENTS WITH A BREAST REDUCTION
A.J., Age 28
Height: 5’2″
Weight: 147 lbs
Right Breast Tissue Removed: 367 g
Left Breast Tissue Removed: 464 g
Before, 6 weeks after
T.L., Age 32
Height: 5’5
Weight: 166 lbs
Right Breast Tissue Removed: 590 g
Left Breast Tissue Removed: 478 g
Before, 3 months, 9 years after
L.M., Age 37
Height: 5’0″
Weight: 194 lbs
Right Breast Tissue Removed: 577 g
Left Breast Tissue Removed: 700 g
Before, 4 months after
J.M., Age 37
Height: 5’0″
Weight: 194 lbs
Right Breast Tissue Removed 541 g
Left Breast Tissue Removed 543 g
Before, 3.5 months after
A.S., Age 38
Height: 5’4″
Weight: 183 lbs
Right Breast Tissue Removed: 314 g
Left Breast Tissue Removed: 181 g
Before, 3 months after
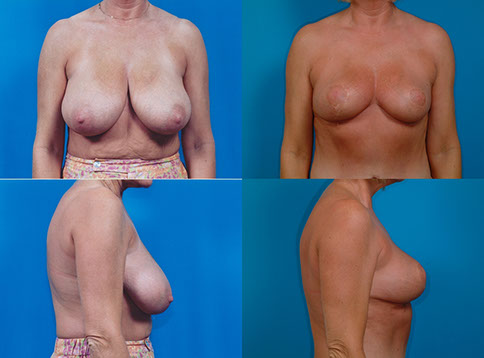
V.T., Age 43
Height: 5’3″
Weight: 161 lbs
Right Breast Tissue Removed: 953 g
Left Breast Tissue Removed: 1040 g
Before, 6 months after
S.S., Age 44
Height: 5’4″
Weight: 186 lbs
Right Breast Tissue Removed: 588 g
Left Breast Tissue Removed: 595 g
Before, 2 years after
D.B., Age 47
Height: 5’2″
Weight: 111 lbs
Right Breast Tissue Removed: 328 g
Left Breast Tissue Removed: 373 g
Before, 3 years after
D.K., Age 51
Height: 5’8
Weight: 190 lbs
Right Breast Tissue Removed: 504 g
Left Breast Tissue Removed: 502g
Before, 3.5 months after
FW., Age 55
Breast reduction, abdominoplasty, and liposuction of abdomen, flanks and inner thighs, and buttock fat injection.
PHOTOS OF PATIENTS WITH A BREAST REDUCTION PLUS IMPLANTS
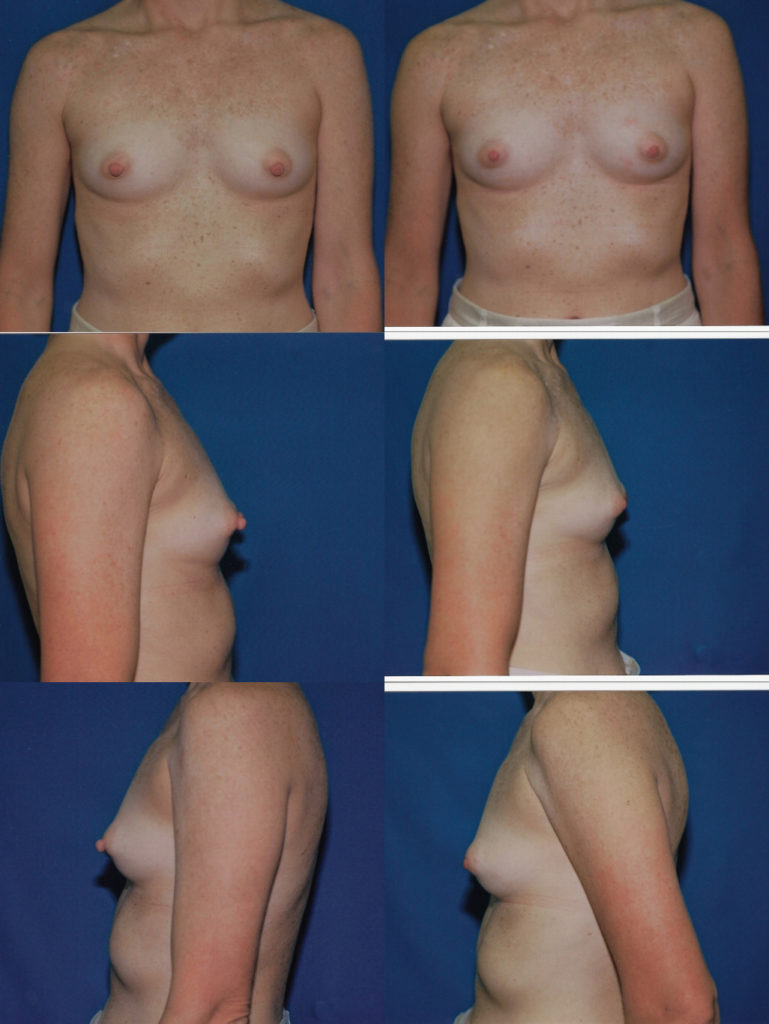
A.V., Age 23
Height: 5’4″
Weight: 116 lbs
Right Breast Tissue Removed: 466 g
Left Breast Tissue Removed: 314 g
Implant Type: Mentor smooth, round, moderate-plus profile, saline
Implant Size: 240 cc
Before, 3 months after
Breast Reduction Plus Implants, Abdominoplasty, Liposuction
L.S., Age 58
Height: 5’6″
Weight: 230 lbs
Placement: Submuscular
Approach: Inframammary
Implant Size: Right Breast: 210 cc/Left Breast: 210 cc
Saline Implants
Before, 3 months after
D.D., Age 59
Height: 5’10”
Weight: 155lbs
Implant Type: Allergan Natrelle smooth, round, moderate profile, saline-filled
Implant Size: 270 cc
Right Breast Tissue Removed: 293 g
Left Breast Tissue Removed: 309 g
Before, 9 months after
PHOTOS OF PATIENTS OVER 50
J.S., Age 50
Height: 5’3″
Weight: 148 lbs
Right Breast Tissue Removed: 547 g
Left Breast Tissue Removed: 480 g
Before, 3 months after
L.M., Age 63
Height: 5’3″
Weight: 135.5 lbs
Right Breast Tissue Removed: 278 g
Left Breast Tissue Removed: 352 g
Before, 3 months after
D.K., Age 51
Height: 5’8
Weight: 190 lbs
Right Breast Tissue Removed: 504 g
Left Breast Tissue Removed: 502g
Before, 3.5 months after
FW., Age 55
Breast reduction, abdominoplasty, and liposuction of abdomen, flanks and inner thighs, and buttock fat injection.
3 Months After
PHOTOS OF PATIENTS WITH REMOVAL OF EXTRA BREAST TISSUE IN THE AXILLAE (ARMPITS)
N.J., Age
Procedure: Removal of breast tissue in axillae
Height: 5’8″
Weight: 170 lbs
Before, 5 weeks
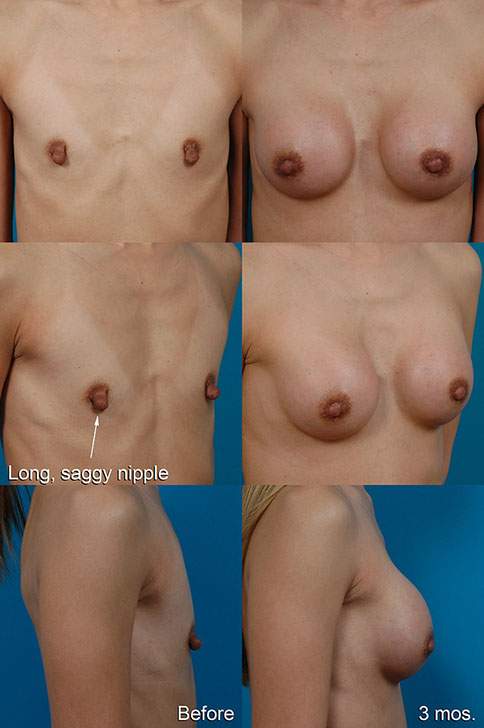
PHOTOS OF PATIENTS WITH NIPPLE REDUCTION
L.L., Age 37
Height: 5’7″
Weight: 130 lbs
This patient’s problem was large, protruding nipples, not large breasts. She had always been self-conscious about her nipples. She was an avid golfer and said that she often wore padded bras just to hide her nipples. Her nipple reduction was performed under local anesthesia, using absorbable sutures. A ring of excess tissue was removed around the base of each nipple, preserving the end of the nipple and its attachments in a central stalk. She reported no pain and was back golfing within 10 days. She was pleased that her nipples were no longer so conspicuous in clothing. This patient would have been well-served with a breast augmentation.
After, 1 month
Over projecting Nipples
J.V., Age 40
Height: 5’2″
Weight: 84 lbs.
Implant Type: Mentor smooth, round, moderate-plus profile, saline-filled
Placement: Submuscular
Approach: Trans-Nipple
Implant Size: 270 cc
Before, 3 months after
Close-up of incision
How It Is Done
The Proper Technique
While there may be a handful of approaches to doing a breast augmentation, there are about 100 techniques described over the years for breast reduction. Few have been subjected to rigorous evaluation with measurements. We know now that the vertical technique fares better than the alternatives in terms of projection, upper pole projection, and aesthetic lower poles.
Can Breasts Be Reduced by Liposuction Alone?
Yes. In fact, for about half my male patients, this is the procedure of choice. However, using liposuction alone there is no removal of extra skin. Skin contraction is limited, so the trade-off is no scars but a looser skin envelope. Most women would rather not have a saggy breast after surgery, even if this means accepting more scars on the skin. A tight, perky breast with a shape more reminiscent of her appearance before the effects of pregnancy and gravity over the years is a worthwhile justification for the scars.
Importance of Technique
There are tremendous differences in how breast reduction surgery is performed, the operative setting, the length of surgery, and operator preferences. When a patient tells me, “My sister had a breast reduction and …,” invariably I have to address misconceptions. Information passed from one patient to another or picked up online may inaccurately color her perception of what to expect. I find myself explaining the technical improvements that make this a patient-friendly procedure. In fact our breast reduction patients experience less discomfort after surgery than our breast augmentation patients do and recover almost as quickly.
This is not an operation for a surgeon who does not have extensive plastic (and especially cosmetic) surgical training, or one who performs this surgery only once or twice a year. Expert judgment is necessary to obtain excellent results. There is little leeway for error, and technique matters. Surgeons often say at meetings that an excellent result can be obtained with a variety of techniques. I have always found this statement counterintuitive and it certainly does not apply to cosmetic breast surgery. Technically proficient surgeons using invalid techniques can expect to have mediocre outcomes.
Attention to blood supply is critical. If the surgeon overdissects, the tissue will not survive. It is possible for part or all of the nipple or large areas of skin to be lost, necessitating additional surgery. An experienced surgeon, who has likely seen and treated this complication, is very attentive to maintaining blood supply to the tissues during surgery, particularly the pedicle supporting the nipple. Surgical times should less than 3 hours. Blood transfusions should rarely be needed. There is no need for the patient to donate blood (“autologous blood”) for administration during surgery. Although this operation was traditionally done in hospitals in the past, most plastic surgeons now perform breast reductions as outpatient procedures. There is no need for drains. A dilute solution containing local anesthetic and epinephrine is injected into the breast tissue to reduce blood loss.
Breast Reduction vs. Breast Lift
A breast reduction is the same operation as a breast lift, except that more breast tissue is removed. All breast reductions are also breast lifts, and all breast lifts are also breast reductions, although small reductions. The incisions are the same. The distinction between the two simply depends on what arbitrary weight of tissue removed is considered a reduction. A small volume of breast tissue may be removed in those patients who desire a lift with a minimal reduction. Alternatively, large volumes may be removed in those patients desiring a significant reduction in size. If the resection weight is less than 300 grams, I regard the procedure as a lift. When I remove more than 300 grams from at least one breast, I consider it a breast reduction. The average resection volume in my practice is about 525 grams per side, but occasionally I remove over 1000 grams per side.
SAFE Anesthesia
The surgery is done under a total intravenous anesthetic, using a laryngeal mask airway (LMA), with no intubation, paralysis, gas, or mechanical ventilation. I call this “SAFE” anesthesia (Spontaneous breathing, Avoid gas, Face up, Extremities mobile). Because patients are not ventilated, paralysis is unnecessary. Patients breathe on their own, with oxygen supplementation. Inhaled gas is avoided. The surgery usually takes 2 hours and patients go home the same day after spending about 1 hour in the recovery room. This type of anesthesia maximizes patient comfort and safety, and reduces recovery time. Because anesthetic gas is avoided and intravenous narcotics are minimized, and anti-nausea medications are given, there is little risk of nausea, which surveys show is the most common patient complaint after surgery in general.
Present-day breast reduction surgery calls for tailored anesthesia, rational procedure selection, limited operating time, negligible blood loss, same-day surgery, and a quick recovery. This represents a major shift from the past model that considered breast reduction a lengthy, onerous procedure, with major tissue dissection, performed in hospitals under a traditional general endotracheal anesthetic.
Antibiotics
Although plastic surgeons have traditionally given antibiotics after surgery, usually for several days, present recommendations are that prophylactic antibiotics should not be continued more than 24 hours after surgery. Longer courses offer no benefit and may cause problems, including a potentially severe form of antibiotic-resistant diarrhea (pseudomembranous colitis), troublesome yeast infections, and the emergence of antibiotic-resistant bacteria such as MRSA.
What To Expect After Surgery
*Swanson E. Prospective outcome study of 106 cases of vertical mastopexy, augmentation/mastopexy, and breast reduction. J Plast Reconstr Aesthet Surg. 2013;66:937–949.
Breast Reduction and Implants
It sounds almost like a contradiction to perform a breast reduction and also use breast implants. Patients might reasonable think, “Doc, my breasts are too big already. Why would I want breast implants?” But patients readily understand that a breast reduction on its own cannot be expected to provide much improvement in upper pole fullness. Repackaging breast tissue in an effort to restore fullness of the upper poles simply does not work. If patients want youthful, convex upper poles without having to rely on a bra, they may consider having small implants inserted simultaneously at the time of their breast reduction. The breasts can still be substantially smaller and not as heavy as they were, but with more volume where it is desirable and much less where it is not. This is an application of the same minus-plus principle discussed previously in the section on breast lifts with implants.
I investigated this topic in a clinical research study comparing women who underwent breast reduction with and without breast implants. All surveyed patients who had simultaneous implants reported that they were pleased with their decision. Physical symptoms were relieved in both groups. The implants did not appear to compromise the physical benefit. Patient satisfaction was > 90% for both groups and patients in both groups reported an improved quality of life. (Swanson E. Breast reduction versus breast reduction plus implants: A comparative study with measurements and outcomes. Plast Reconstr Surg Glob Open 2014;2:e281.) This study won Best North American Paper published in PRS-GO for the year 2014.
Recovery
Patients are often pleasantly surprised that there is not as much discomfort as they expected after a breast reduction. Usually, there is not a great deal of pain with this procedure. In fact, the average pain rating is only 3.3/10.
Patients take painkillers for 5 days, on average, are back to work in 8 days, and report feeling “back to normal” in 1 month.
I do not use drains in performing breast surgery. The dressings come off when the patient returns to the office on the day after surgery. Patients may then start bathing right away. The incisions are covered by small semi-transparent adhesive strips (“Steri-Strips”) which stay on even during bathing. A light gauze dressing is inserted in the bra for comfort and to collect small amounts of fluid which ooze from the wound. This tissue fluid usually stains the gauze yellow and is normal. The Steri-Strips come off at the second office visit, usually 1 week later. Sometimes they start to peel off sooner, and that is okay. They are an extra precaution and are not even used in patients who are allergic to them. The soft sports bra is worn day and night for 1 month, and then according to patient comfort, on during the day and off at night. Underwire bras are to be avoided for at least 1 month to avoid any undue pressure on the incisions while they are healing. A moisturizer may be used to treat dry skin. A topical antibiotic such as Neosporin is used to treat any areas of crusting or delayed healing after the Steri-Strips come off.
Swelling
The breasts swell right after surgery. They may feel tight and look unnatural —flat across the bottom rather than rounded, with excessive upper fullness and an indistinct cleavage. This is due to swelling and skin tightness. These findings are expected. Gradually the swelling dissipates and the tissue relaxes. Over the next few months, the breasts will settle and look more pendulous and natural. Bruising can take several weeks to clear.
Numbness
Because the skin is cut during the procedure, small sensory nerve branches in the skin are divided. Gradually these tiny nerve endings regenerate and the feeling gradually returns. Nipple sensation usually remains intact, because the nerves that supply it from below are preserved. (The surrounding skin is removed while the nipple itself stays attached to the underlying breast tissue). However there may be loss of feeling in the nipples, usually temporary.
Activity
Although the usual time period off work is one week, many women resume working after three or four days, provided they have a sedentary job. Jobs requiring physical activity (waitress, factory worker, etc.) will have longer recovery times, up to three weeks. Women can walk right away, and walk a few miles, to maintain fitness about two weeks after surgery. Exercise involving upper body activities should be avoided for one month, when patients may resume full physical activity.
Scarring
Like all scars, particularly on the body (as opposed to the face where scars generally heal well), breast scars may widen. There is certainly a genetic component to this, and clues may be obtained from other scars on the body, especially the abdomen. How did the appendectomy or Caesarean section scar turn out? If a patient has a nicely healed and inconspicuous abdominal scar, chances are their breast scars will do well too. However, if they heal with thick, raised hypertrophic scars or are prone to keloids, their breast scars are likely to be similarly affected. In this situation, it may be best not to have the surgery—the balance is too much on the cost side (significant scars) and not enough on the reward side (improved breast shape).
Surgery creates some tension on the scars. This tends to make them widen. Later, when the tension has reduced by relaxation of the tissues, the scars may be revised, if necessary, usually under local anesthesia.
Scarring and the Older “Inverted-T” Technique
The horizontal scars left by the older inverted-T technique had the most problem with such scars. These scars could be seen close to the midline and on the side where they were not always hidden under the breast crease. Patients find these scars the most objectionable of the three scars (periareolar, vertical, and horizontal) that are part of the old inverted-T anchor incision. This is one reason why it is so much better to avoid using the inverted-T technique.
Vertical Scar Healing
The vertical scar often heals nicely, although it is not unusual to have small areas of delayed healing. If it needs to be revised, because of an excessively wide scar, this may often be done under local anesthesia.
Puckering or “Dog Ears” and Scarring
There is a pucker (“dog ear”) at the bottom of the vertical scar. This is created when an ellipse of tissue is removed above it. The only way to avoid such puckering is by making the incision longer. Of course, we don’t want to do this because we want to limit the length of the incision so as not to leave a scar continuing down on the abdomen. By removing the breast and fat tissue deep to the lower end of the scar, this helps to allow the puckering to settle down. However, it is sometimes necessary to come back and treat a persistent dog ear by cutting out a small area of puckering that does not completely flatten out. It is not unusual for me to use a small inverted-T at the bottom to keep the scar from extending onto the abdomen. This is a much shorter scar than the horizontal component of the traditional inverted-T anchor scar. Even with diligent surgery and follow-up care, scars may widen. But they will look better with time. They will soften and the redness will gradually fade.
Complications
Persistent Lower Pole Fullness
This is the most common complication of a breast lift or reduction. It is usually caused by inadequate removal of breast tissue from the lower pole of the breast, so that there is a persistent bulge of the lower pole, which one surgeon (Flowers) colorfully calls the “mastopexy-wrecking bulge.” This problem is common among patients treated with “skin-only mastopexies” because the skin stretches readily and cannot hold the breast shape. It is also commonly found in patients treated with “periareolar” or “donut” mastopexies because these techniques do not allow removal of breast tissue from the lower pole. They do avoid a vertical scar, leaving just the scar around the areola, which is the appeal of these limited-incision techniques, but this benefit is outweighed by the inability of these techniques to adequately tighten the lower pole and provide a lift. The vertical method provides the best breast elevation and the most conical (“tight”) lower pole shape. (Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128:1282–1301.)
Infection
As in any surgery, infection is a risk. Patients take antibiotics for 24 hours, starting on the day of surgery. They start bathing as soon as the dressings come off.
Hematoma
A hematoma is signaled by marked discomfort and swelling, usually on one side, almost always occurring within the first 24 hours after surgery. Recognition is the key. If the patient returns to the operating room promptly for treatment, she is unlikely to have any problems from this.
J.S., Age 50, Self-Employed
Height: 5’3″
Weight: 148
Children: 2
Right Breast Tissue Removed: 547 g
Left Breast Tissue Removed: 480 g
Preop. Bra Size: 38DD
Postop. Bra Size: 38C
Comments: This patient developed increased discomfort, swelling, and bruising of the left breast. She returned to the operating room for treatment of a hematoma. These photos also show the early puckering and bruising at the bottom ends of the vertical incisions. This puckering (“dog ear”) usually settles down on its own within 3 months of surgery.
Before, 2 days after, 3 months after
Skin Loss/ Delayed Healing
Because skin circulation is partially interrupted by raising skin flaps, avoidance of smoking is important to reduce the risk of loss of skin along the wound margins. This is true in any procedure which involves raising skin flaps (facelift, abdominoplasty, and breast lift/reduction). If some loss along the wound edge does occur, the patient is reassured and instructed to keep the open area clean with soap and water, apply antibiotic ointment and a light gauze dressing. The wound is allowed to heal in on its own. Because wounds contract in from the sides and shrink as they heal, the resulting scar is often surprisingly small, and usually requires no treatment. Scars that widen as they heal may be treated later with a scar revision. The vertical technique has an advantage because thin skin flaps are avoided and the risk is reduced.
Although rare, it is possible to lose portions, or all, of the areola and nipple. Anything that interferes with circulation to the skin such as excessive tightness, an underlying hematoma, pressure on the skin, or smoking (due to nicotine), can lead to this complication, which is obviously best avoided. Smoking cessation patches and gum also contain nicotine, the substance which causes the small blood vessels to tighten, so these also need to be avoided.
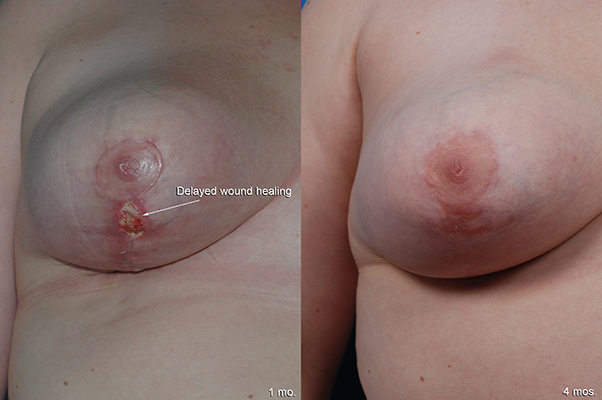
Delayed Healing After Breast Reduction
A.C., Age 26, Teacher
Height: 5’3″
Weight: 174
Children: 0
Right Breast Tissue Removed: 410 g
Left Breast Tissue Removed: 612 g
Preop Bra Size: DD
Postop. Bra Size: C
Comments: This patient is seen 1 month and 4 months after a breast reduction. An opening developed just below her right areola, called a partial wound dehiscence. The patient was reassured and instructed to keep the wound clean and allow it to heal on its own. Often, such areas of delayed healing along the vertical incision line heal well on their own, so that a scar revision is often unnecessary. Note the improved breast projection on the lateral view.
1 month after, 4 months after
Before, 4 months after
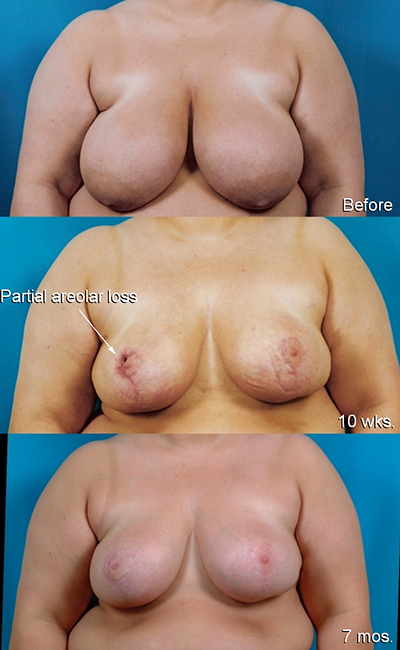
Partial Loss of Areola After Breast Reduction
L.B., Age 29, Executive Recruiter
Height: 5’6″
Weight: 253
Children: 0
Right Breast Tissue Removed: 738 g
Left Breast Tissue Removed: 744 g
Comments: This 29-year-old obese nonsmoker developed loss (necrosis) of a portion of her right areola after a breast reduction. This wound was treated with dressing changes and went on to heal with an acceptable scar. No revision was necessary.
Before, 10 weeks after, 7 months after
Deep Venous Thrombosis
A blood clot can sometimes develop after surgery, affecting a leg vein. It is important to detect any clots early, while they are small, so that blood thinners can be prescribed to help them dissolve. To reduce risk, surgery is done under total intravenous sedation without muscle relaxation to avoid blood pooling in the calves. In addition, ultrasound screening is routinely performed to detect early blood clots that might develop after surgery.
Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96.
Care After Surgery
The incisions drain a yellowish fluid and a small amount of blood for several days after surgery. Use gauze inserts in your bra to collect this fluid and change as necessary at least twice a day. Leave your dressing on and keep it dry until you are seen by the doctor for your first follow-up appointment, usually the day after surgery.
The local anesthetic works for several hours. Your breasts will start to get sore on the evening after surgery. Take one painkiller every 4 hours as necessary. You can take two at one time if needed. Be sure to take the medication with a light snack—crackers or toast. Ibuprofen or acetaminophen may be used as an alternative to the prescription painkillers if the pain is not too severe. Non-steroidal anti-inflammatories avoid the side effects of narcotic painkillers, such as constipation, nausea, and sedation. Be sure not to exceed the maximum recommended dose (4000 mg/day for acetaminophen or 3200 mg/day for ibuprofen).
It is normal for your breasts to be swollen, sore and bruised. At first they appear flattened across the bottom. Gradually, your breasts will look more natural and the contours will start to round out over the next few months. The swelling and soreness take up to a month to resolve, but most of it goes away in the first 2 weeks. Notify the doctor if one breast becomes much more swollen, painful, tight or bruised than the other. This could indicate a hematoma (postoperative bleeding) that needs prompt attention. A hematoma rarely occurs more than 24 hours after surgery. For this reason, we insist that out-of-town patients stay in the area at least overnight and are seen in follow-up the next day before returning home.
At the time of your follow-up appointment at the office, the dressings are removed. The semitransparent tapes on the skin (Steri-Strips) are left on and your bra is put back on with gauze inserts. You can replace the gauze pads as necessary. It is now okay to start bathing. If any of the Steri-Strips come off in the water, that’s okay. Wear the bra both day and night for 2 weeks for comfort and protection. Lie on your back to sleep. Avoid lying on your tummy or side for a few weeks until this becomes comfortable. Allow at least 1 month before sleeping on your tummy.
It is okay to wear a sports bra instead of the garment provided at the time of surgery. Because of the pressure from the wire, avoid wearing underwire bras for 1 month so there is no undue pressure on the incision.
Avoid vigorous exercise for at least 2 weeks after surgery. Avoid heavy lifting (more than 20 pounds) during the first week after surgery. Postpone doing heavy housework, mowing the lawn, or lifting heavy bags of groceries for at least 2 weeks.
You may resume exercise gradually, performing light cardiovascular exercises 2 weeks after surgery, such as walking on a treadmill. Full aerobic exercise may be resumed 1 month after surgery. Keep in mind that everyone heals at a different pace. Your body will tell you (with pain and swelling) when you are overdoing it.
A low-grade fever (under 101° F or 38.5°C) is normal during the first 48 hours. Report any persistent fever, increasing rather than decreasing pain or swelling, or any malodorous drainage from the incision. Blood-tinged or yellowish drainage is normal.
Most women are able to return to work 1 week after surgery. If you have a more physical job (server, nurse, factory worker), a period of at least 2 weeks is recommended. Remember that you will be sore for about 1 month.
Wait until the bruising is gone before using a tanning bed (which of course is not recommended). Protect the incisions from ultraviolet light with a bikini top and sunblock. The incisions will heal with a less conspicuous scar if they are protected from UV exposure for at least 6 months. Ultraviolet light can make them darken (“hyperpigmentation”).
The stitches dissolve on their own. Sometimes suture ends that become exposed are trimmed by your surgeon or assistant at the time of your follow-up visit. Antibiotic ointment such as Polysporin or Neosporin may be applied to any open areas or crusts, twice a day.
FAQ’s
Q: How much work will I miss?
A: As with any surgery, there is a range. Our patients reported being off work from 2–20 days. But the average period off work was 8 days.
Q: What is recovery like?
A: The average pain level is quite modest—only 3.3 on a scale of 1–10. The recovery after a breast reduction is usually easier than patients expect.
Q: Does it matter if I’m a smoker?
A: Nicotine interferes with skin circulation, raising the risk of delayed healing, skin necrosis and even nipple/areola loss. However, the vertical technique avoids skin undermining and uses a short, superficial pedicle, making it more robust so that smokers can be treated. But it is still best to avoid smoking to make the surgery as safe as possible.
Q: Will I sag again?
A: With time, you will experience natural sagging. Gravity will continue to exert its effect of course. Pregnancy and changes in your weight could also contribute to sagging. If you have breast implants at the same time you may have better long term results. I typically make patients as “perky” as I can, knowing that gravity will eventually cause them to settle down.
Q: How long does this surgery take?
A: You’ll be in surgery about 2 hours.
Q: Do you use drains?
A: No.
Q: Do you use the anchor scar (inverted-T) technique?
A: No, I prefer the vertical technique because of its multiple advantages in terms of safety, aesthetic result, nipple sensation, and suitability when implants are used simultaneously. This method frequently includes a horizontal scar in the crease under the breast, but the scar is not as long as the anchor scar.
Q: What happens to the feeling in my nipples?
A: There may be a temporary loss of sensation, but this feeling usually returns. The nipples maintain their attachment to the underlying tissue and to the skin on the medial side. Important sensory nerves supplying the nipples from below and the medial side are left intact, so that nipple sensation is usually preserved.
Q: How bad are the scars?
A: The scars are better with the vertical technique compared with the anchor scar.. A long horizontal scar extending almost to the midline and around the side is avoided. The scars usually heal well and are well-concealed.
Q: Can I still breastfeed?
A: Because the nipple stays attached to the underlying breast tissue, this surgery is unlikely to affect your ability to breastfeed.
Q: Should I have a mammogram first?
A: Recommendations regarding mammograms do change from time to time and it is best to defer to the advice of your primary physician. If you are due for a mammogram, have it done before your breast reduction. You can have mammograms after the breast reduction, but it is best to schedule this at least 6 months after your breast augmentation, unless there is a medical reason (like a lump) to do so earlier.
Q: When can I return to work?
A: Most patients return to work in a week, but there certainly is a range. Some women get back to work in a few days and others are glad they took a week off. If you have a physical job, 2 to 3 weeks off is better.