INTRODUCTION
What Is the Ideal Body?
In centuries past, the female form has been somewhat heavy in many cultures, a sign of health and nutrition. This full form has given way in the last few decades to a lean look, albeit with full breasts. This combination is unusual in nature. Few women are naturally endowed with an enviable lean physique and full breasts. Similarly, few men are endowed with the physique of Michelangelo’s David, who did not have “love handles”!
What Are Healthy Body Proportions?
Healthy premenopausal women have waist-to-hip ratios of 0.67 to 0.80. This means that their waist circumferences are seven to eight-tenths as large as their hips. A healthy man’s waist-to-hip ratio is between 0.85 and 0.95. Moderate weight gain does not alter these basic male and female shapes, and they are found all over the world among people who vary considerably in height and weight.
Men have an innate preference for female bodies with narrow waists and full hips, which signal high fertility, high estrogen, and low testosterone. Cartoon characters and virtual images of females like Jessica Rabbit (Who Framed Roger Rabbit, 1988) and Lara Croft typically have exaggerated proportions. Barbie (at least the original Barbie) has measurements of 36-18-33, with a 0.54 waist-to-hip ratio. Audrey Hepburn and Marilyn Monroe represented two different images of in the 1950s. Yet, the 36-24-34 Marilyn and the 31.5-22-31 Audrey both had versions of the hourglass shape and waist-to-hip ratios of 0.70. During the 20th century, Miss America and Playboy centerfolds’ waist-to-hip ratios measurements ranged from 0.68 to 0.72. By the end of the 20th century, the average supermodel measured 33-23-33, giving her a 0.70 waist-to-hip ratio.
The Miss Americas of the 1960s were 5’6″ tall and weighed 120 pounds. Twenty years later they had gained 2 inches in height but remained the same weight. Playboy playmates also dropped several pounds and gained several inches in height during the same period, dipping from 11% below the national average to 17% below it. Even the Columbia Pictures logo, the torch-bearing woman, was slimmed in 1992.
Presently, 64% of American adults are overweight, defined as having a body mass index of 25 or greater, and 31% are obese, having a body mass index of 30 or greater.
Body Shape Is Hereditary
It comes as no surprise to most of us that our body shape resembles other family members. Women sometimes refer to the “apple shape” or “pear shape” to describe less than ideal proportions. Our body fat distribution and number of fat cells is determined genetically. By the time we are adults, the number and distribution of fat cells in our body is unchanging. The exception occurs only at extremes of weight. When we gain weight, our existing fat cells swell and when we lose weight they shrink. But, their number and distribution remain the same. This fact explains why we find that our dimensions are reduced after weight loss, and increased with weight gain, but our body proportions stay about the same. Women with a pear shape (also unfavorably compared to a bowling pin) may find that they can drop from a size 8 to a size 6, but jeans are still tight on the thighs and loose at the waist. No amount of exercise and fat burning can overcome genetics. As a consequence of this fact, even professional athletes, body builders, personal trainers and aerobics instructors have liposuction.
Pregnancy and Body Shape
Pregnancy does not permanently alter body fat proportions. The tummy is stretched out, of course, and the body swells during pregnancy, but there is no net gain or loss of fat cells. This fact explains why, after losing their weight after pregnancy, women find that their body shape is unchanged. The abdominal skin and muscles have been stretched, so the skin tone will not be as tight as it was, and there is likely to be some degree of abdominal “pooch” due to stretching of the muscles, but even in the tummy, there is no fat that was not there before.
Achieving Ideal Body Proportions
Our major tool to achieve optimal body proportions is liposuction. As you explore the procedures in this section, you will learn how you can take advantage of body contouring options to enhance your appearance beyond what is possible with a healthy diet and exercise alone.
Adults have a fixed number of fat cells, and the only way to remove these fat cells is by liposuction. This provides permanent correction of body disproportions. Contrary to rumor, any weight gain after surgery is evenly distributed all over the body—it does not return specifically to the treated areas or accumulate instead in untreated areas.
Liposuction and Body Weight
Patients often remark, “I heard that if you have liposuction on the hips and thighs, when you gain weight you’ll gain it in other areas, like your face and your arms.” This is not true. Think of it this way: the rest of the body does not know that their fat cell neighbors in the love handles have “left the building.” Their size is simply determined by how many calories get delivered to them. They will swell if the body consumes more calories than it burns, or shrink if the body burns more calories than it takes in.
Does the Fat Come Back?
An article that was published in the Obesity Journal in 2011 suggested that fat removed by liposuction of the lower body returns later to the upper body, making women look disproportionate. An illustration in the New York Times showed a drawing of a woman looking like the Incredible Hulk after liposuction. No woman wants to trade lower body fat for upper body fat. There were a number of problems with the study including weight gain by subjects, inaccurate measurement techniques, small patient numbers and nonsignificant findings. In addition, there is no known physiological basis for such a fat redistribution mechanism. Rigorous photometric analysis reveals no distribution of fat (Swanson E. Photographic measurements in 301 cases of liposuction and abdominoplasty reveal fat reduction without redistribution. Plast Reconstr Surg. 2012;130:311e–322e; discussion 323e–324e). Measurements showed long-term improvement in body proportions after liposuction and tummy tucks with no subsequent fat accumulation in treated or untreated areas.
So, how does a rumor like this get started? One possible explanation is that people rely on their clothes as a guide to when to cut back on calories. After liposuction, their clothes fit more loosely because fat cells in these areas have dearly departed. So it is possible that they may gain weight until they fit clothes like they did before. Only now they are fuller in other parts of the body that were not reduced with liposuction, like the face and arms.
These patients see me in follow-up and say, “Doctor, I’m disappointed. I really didn’t notice that big of a difference after liposuction.” Before any further discussion, these patients are asked to step on the scales. Invariably, they weigh more, sometimes 10 pounds more, than they did at the time of liposuction. Of course, they should weigh less, not more, because the fat that was removed at surgery weighed several pounds, and sometimes as much as 10 pounds. Patients are invariably surprised when they learn of this weight gain.
So the patient has actually gained weight since the surgery, compromising their reduction from liposuction. In fact, if they had not had liposuction, they would likely not be able to fit into their pants. Patients ask, how did I gain that weight? Likely they gained weight because they were less active, but continued eating the same way. More calories, less exercise equals weight gain. Plus, their usual “alarm”—tight fitting clothes—did not alert them to cut back.
Fortunately, the outcome can still be a favorable one. Because the number of fat cells is fixed, there is no permanent harm done by temporary swelling of the fat cells. But, the patient needs to return to full activity and proper diet. When the weight returns to normal (the same as at the time of surgery or less), the patient will better appreciate the results of liposuction. With good behavior, the result just gets better and better.
I usually take photographs at least 3 months after liposuction. This allows enough time for the swelling to go down fully. Ideally, the patient will weigh the same as what they did on the day of surgery, or even a little less, accounting for the volume of fat removed by liposuction. This is about 2 pounds per liter. So if a patient had 3 liters (3000 cc) of fat removed by liposuction, she should weigh 6 pounds less when the swelling has gone down. Therefore, to appreciate the results of liposuction without any compromise due to postoperative weight gain or loss, this patient should weigh 6 pounds less than on the day of surgery, when the postoperative photographs are taken.
Liposuction and Fat Cell Removal
Another popular misconception surrounding liposuction: “If I gain weight it will just come back and I will have wasted my time and money having liposuction.”
Certainly, if any benefit realized by liposuction was lost the next time we put on 5 pounds, there would be no point in having liposuction in the first place. But, the results are still there at the heavier weight. The patient will always fit into her clothes better than she would have without liposuction, regardless of how much she weighs, for the rest of her life because there are fewer fat cells in the treated areas. And when she loses the 5 pounds, her shape returns to what it was right after liposuction. In fact, it is impossible to lose the benefit of liposuction, even if she wanted to do so, barring extreme weight gain. (At extreme weight the fat cells reach the limit of their capacity to expand and will start making new fat cells to hold the additional fat.)
Patients sometimes look at me with a degree of skepticism when I explain this, but they need only look at long-term results to see that this is true. They understand the concept once they understand that fat cell numbers are genetically determined and do not change during weight gain or loss. The only way to change fat cell distribution is by physically removing them using liposuction (or adding by fat injection). Liposuction permanently improves body proportions. This capability is the reason liposuction has been the most popular cosmetic operation of the last couple of decades.
Most patients are attentive to diet and exercise after surgery and lose rather than gain weight. By correcting body disproportions, patients experience a psychological benefit, and find that they are better motivated to maintain their improved body form.
Obese Patients
Although liposuction has been used to treat obesity, it is now recognized that this is not the best application of liposuction. In very obese patients, the volume of fat and fluid removed may be much larger (well over 5 liters), making fluid management more difficult, and increasing the risk. Furthermore, the difference in body contours is proportionately less, making the procedure less worthwhile. Also, these patients have not developed good eating habits and exercise regimens (obesity speaks for itself) so that they may be more likely to gain weight after surgery, particularly if they are even less active.
Beer Bellies
Patients with a “beer belly” are the worst candidates for liposuction. These patients have very protuberant abdomens, but there is minimal subcutaneous fat. There is not much surface fat to grab. Almost all the fat is on the inside the abdomen (“intraperitoneal”), wrapped around the organs and therefore inaccessible to liposuction. These patients are understandably disappointed, but are sorted out early in the consultation. They are glad to be told candidly that they are not good candidates so they do not waste their time and money having a procedure that is unlikely to help much. I recommend professional weight loss counseling. Dieting and weight loss is the only way to reduce a beer belly.
Health Benefits—Reduced Triglycerides and White Blood Cell Count
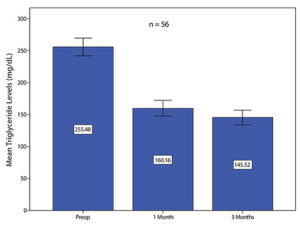
Patients sometimes ask if there are any long-term health risks associated with liposuction. For example, how does it affect cholesterol levels? Liposuction has no effect on cholesterol levels (Swanson E. Prospective clinical study reveals significant reduction in triglyceride level and white cell count after liposuction and abdominoplasty and no change in cholesterol levels. Plast Reconstr Surg. 2011;128:182e–197e). This finding is not surprising because fat cells do not manufacture cholesterol. However, they do contain triglycerides. People with high triglyceride levels experience a 43% drop in triglyceride levels, on average. A surprising and unexpected study finding was that white blood cell counts are reduced 11% on average after liposuction. Although there are no studies to indicate that these favorable changes are associated with health benefits, there is evidence that high triglyceride levels and high white blood cell counts are unhealthy, so the news is welcome.
Triglyceride levels in liposuction patients with preoperative levels greater than or equal to 150 mg/dl. Both 1-month and 3-month mean triglyceride levels are significantly lower than the mean preoperative level (p < 0.001). The mean decrease 3 months after liposuction is 43%.
How Effective Is Liposuction?
Liposuction has been used for over 35 years now. Surprisingly, its effect on the thickness of the fat layer was only recently determined (Swanson E. Assessment of reduction in subcutaneous fat thickness after liposuction using magnetic resonance imaging. J Plast Reconstr Aesthet Surg. 2012;65:128–130) using magnetic resonance imaging. See illustration below:
This 24-year-old study participant’s (above) photographs and (below) magnetic resonance imaging scans were taken (left) before and (right) 6 months after liposuction of her lower body and breast augmentation. The total aspirate volume was 3000 cc. The subcutaneous fat appears white in these coronal, T1-weighted images. Measurements are indicated at the level of the left flank and outer thigh. The thickness of the abdominal fat pad was also measured, using axial slices (not shown).
On average, the fat thickness is reduced about 45% after liposuction and two-thirds of the swelling is gone by the first month. It takes about 3 months for the swelling to completely resolve. Unlike, for example, breast augmentation and abdominoplasty, the results of liposuction are not immediately apparent after surgery and patience is needed to appreciate the full effect.
What About Coolsculpting?
Coolsculpting, or cryolipolysis, has recently entered the marketplace as a nonsurgical alternative to liposuction. This machine freezes the fat. Proponents concede that the effects are not as dramatic as liposuction. Studies using ultrasound have detected a small difference in the thickness of the fat layer after treatment—a reduction of 1/10 of an inch in 16 weeks. It is time-consuming, expensive, and provides only spot treatments (like LipoDissolve used to do). Investigators generally have financial conflicts. Many owners of these systems report underwhelming results. Unlike liposuction, there is a deficiency of published studies using MRI or photometric analysis to demonstrate its effectiveness
(Swanson E. Cryolipolysis: The importance of scientific evaluation of a new technique. Aesthet Surg J. 2015;35:NP116–NP119).
A troubling complication of crylipolysis is paradoxical adipose hyperplasia (PAH). In some patients, for unknown reasons, this treatment stimulates the formation of new fat cells – the exact opposite of the desired effect. When Coolsculpting was introduced, this complication was thought to be very rare. However, operators have learned that it is not so rare, affecting about 1% of patients. These patients are understandably upset. They chose a nonoperative treatment; now they are forced to have an operation (liposuction) to alleviate this problem.
Liposuction of the Arms: How It Is Done
An incision is made in the armpit. The area is first injected with anesthetic solution, the same way that liposuction is performed in other areas, using the “superwet” technique.. The next step is removal of the fat using liposuction.
Some surgeons have been reluctant to treat the arms or calves because of concerns about complications. However, if the superwet technique is used, incisions are limited, and overtreatment avoided, these become very favorable areas to treat with minimal risk.
History of Liposuction
Advances in liposuction include the evolution of instruments, energy source, wetting solutions used to pretreat the areas, and anesthesia.
Traditional Liposuction (1982)
Instrument: Cannula, large bore
Energy: Physical
Solution: Either none (“dry liposuction”) or small volumes
Results: Small volumes of fat removed, spot treatments, irregularities and blood loss. Liposuction was refined and reintroduced by a French plastic surgeon, Dr. Illouz, in the 1970s. Liposuction started off as basically making an incision and suctioning fat. Sounds simple enough, but this was a big advance in body contouring!
Tumescent Technique (1990)
Instrument: Blunt cannulae, smaller caliber
Energy: Physical
Solutions: Tumescent: saline, lidocaine, epinephrine
Results: Larger volumes of fat removal, multiple areas, smoother borders, less blood loss.
In 1990, an American dermatologist, Dr. Klein, described the tumescent technique. This was a big step forward. The tissues were injected with a large volume of saline solution prior to performing liposuction. This saline solution contained epinephrine, to reduce blood loss, and lidocaine, a local anesthetic. The local anesthetic allowed the procedure to be performed using local anesthetic alone, in the doctor’s office, making it a tool for non-surgeons.
The fluid injected into the tissues served to hydrate the patient during surgery, so that little or no extra I.V. fluid administration was needed. The infusion of fluid into the tissues filled up the tissues, making them “tumescent.” This facilitated liposuction by magnifying the fat layer, helping to make the contours smoother because it was easier for the operator to avoid going too close to the skin or oversuctioning areas, which would cause irregularities.
The epinephrine contained in this fluid greatly reduced blood loss. This enabled the surgeon to treat multiple areas at one time and remove greater quantities of fat. The surgeon was no longer limited to spot treatments. All of the affected areas could be treated simultaneously. Patients could be treated at one setting instead of returning for multiple procedures. The technique had matured and could now deliver worthwhile results for the thousands of people with body contour problems. Its popularity grew and it quickly became the most popular cosmetic operation.
“Laser” Liposuction
Laser systems (example: Smartlipo) use a low-energy laser light beam to break up fat cells. Laser systems are costly and add a price increment to surgery because a non-reusable tip is needed for each patient. Importantly, the laser used in liposuction does not selectively target fat cells. Studies have failed to show a definite advantage for liposuction devices that incorporate a laser. Investigators found greater cellular damage to the fat cells and greater release of triglycerides from laser treatments (versus liposuction without laser pretreatment) and no improvement in skin retraction. The word “laser” has marketing appeal in medicine and the investigators cautioned against “putting commerce before research.”
Radiofrequency-Assisted Liposuction
This method uses a heat probe under the skin to produce coagulation of the fat layer and, in so doing, tighten the skin. However, the treatment introduces complications related to the thermal energy, including the possibility of burns. Like laser liposuction, radiofrequency is not specific for fat cells, and damages other tissues such as nerves and lymphatics. It also adds expense. Many of the publications on this device are affected by conflict of interest – the authors receive financial compensation and free devices. It is not FDA approved for skin tightening. The skin often contracts without using heat under it (as evidenced by this section, Abdominoplasty, and Submental Lipectomy). When considering the pros and cons, it is difficult to make a case for radiofrequency.
Ultrasound Surveillance for Blood Clots
Swanson Center for Cosmetic Surgery is presently engaged in a clinical trial to determine the feasibility and effectiveness of using Doppler ultrasound to screen patients before surgery, the day after surgery, and about 1 week after surgery. This highly accurate and noninvasive method can detect small clots before they grow and become dangerous. The results of ultrasound screening in 1000 consecutive plastic surgery outpatients were published in 2020. The findings were surprising in many ways. First, blood clots rarely formed during surgery. They were usually detected a week after surgery. Clots usually formed in the smaller distal veins of the legs and took about 5 weeks to resolve with treatment (oral anticoagulants). Sequential compression devices were of no clinical benefit. A simultaneous laboratory study showed no fibrinolytic benefit for these devices either. These results support total IV anesthesia and routine ultrasound screening. This method can be used instead of “risk stratification” and “chemoprophylaxis,” which are of questionable effectiveness and can increase the risk of unnecessary postoperative bleeding.
Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96.
Swanson E. The effect of sequential compression devices on fibrinolysis in plastic surgery outpatients: A randomized trial. Plast Reconstr Surg. 2020;145:392–401.
Swanson E. Reconsidering the role of routine anticoagulation for venous thromboembolism (VTE) prevention in plastic surgery. Ann Plast Surg. 2020;85:97–99.
Swanson E. Distal deep vein thrombosis causing pulmonary embolism after outpatient plastic surgery: A case report. Plast Reconstr Surg Glob Open 2020;8:e2803.
Swanson E. Ultrasound surveillance offers a safe and effective method for venous thromboembolism prevention in plastic surgery patients. Aesthetic Plast Surg. 2020;231:783–784.
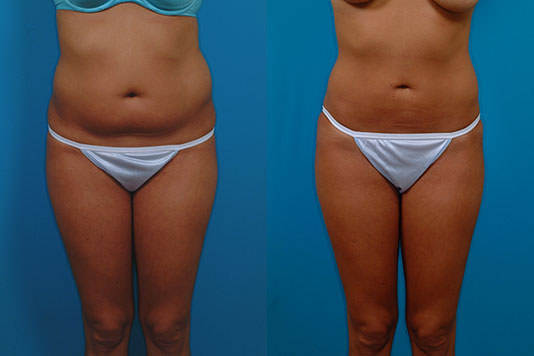
PHOTOS OF FEMALE PATIENTS
M.G., Age 21
Procedure: Liposuction of lower body and submental lipectomy
Before, 2 months after
H.E., Age 22
Procedure: Liposuction of lower body (no knees). Touch-up 1 year later: lower buttocks
Before, 2 years after, 11½ years after
M.C., Age 22
Procedure: Liposuction of abdomen, flanks, inner thighs, arms, and axillae. Submental lipectomy.


Before, 1 year after
J.J., Age 24
Procedure: Liposuction of the abdomen, flanks and axillae

Before, 3 months after
A.M.
Age 25
Liposuction abdomen, flanks, and inner thighs.
3 months
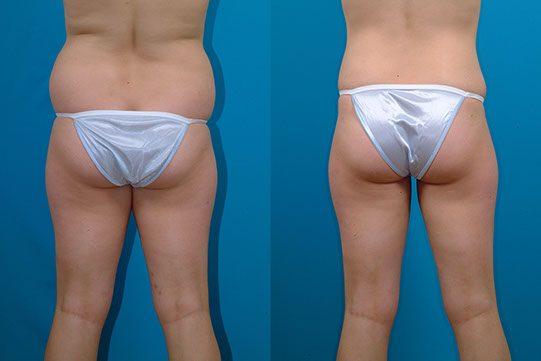
B.S., Age 30
Procedure: Liposuction of abdomen, flanks, and inner thighs, and buttock fat injection.
Before, 1 month after
C.M., Age 31
Procedure: Liposuction of abdomen and flanks
Before, 6½ months after
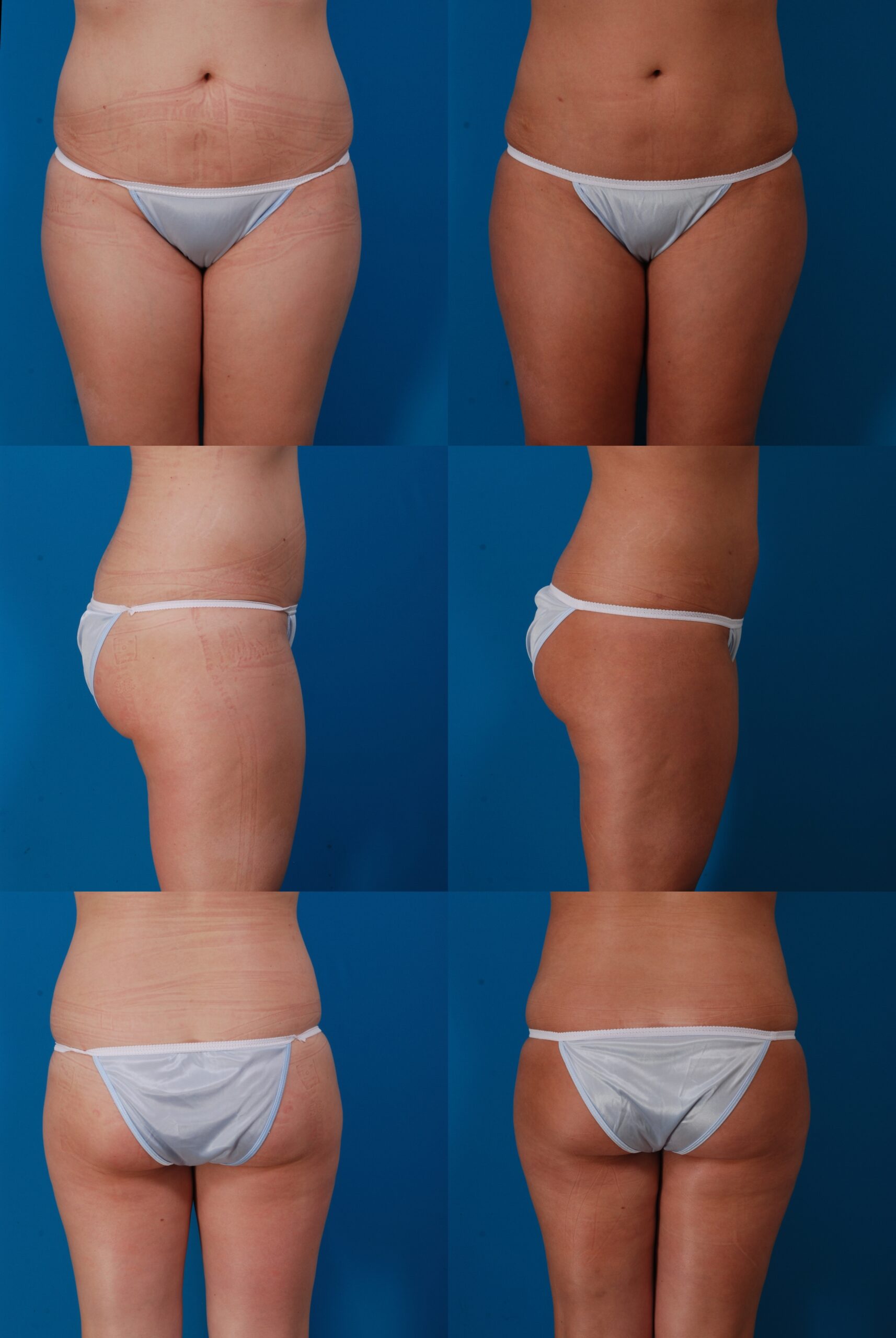
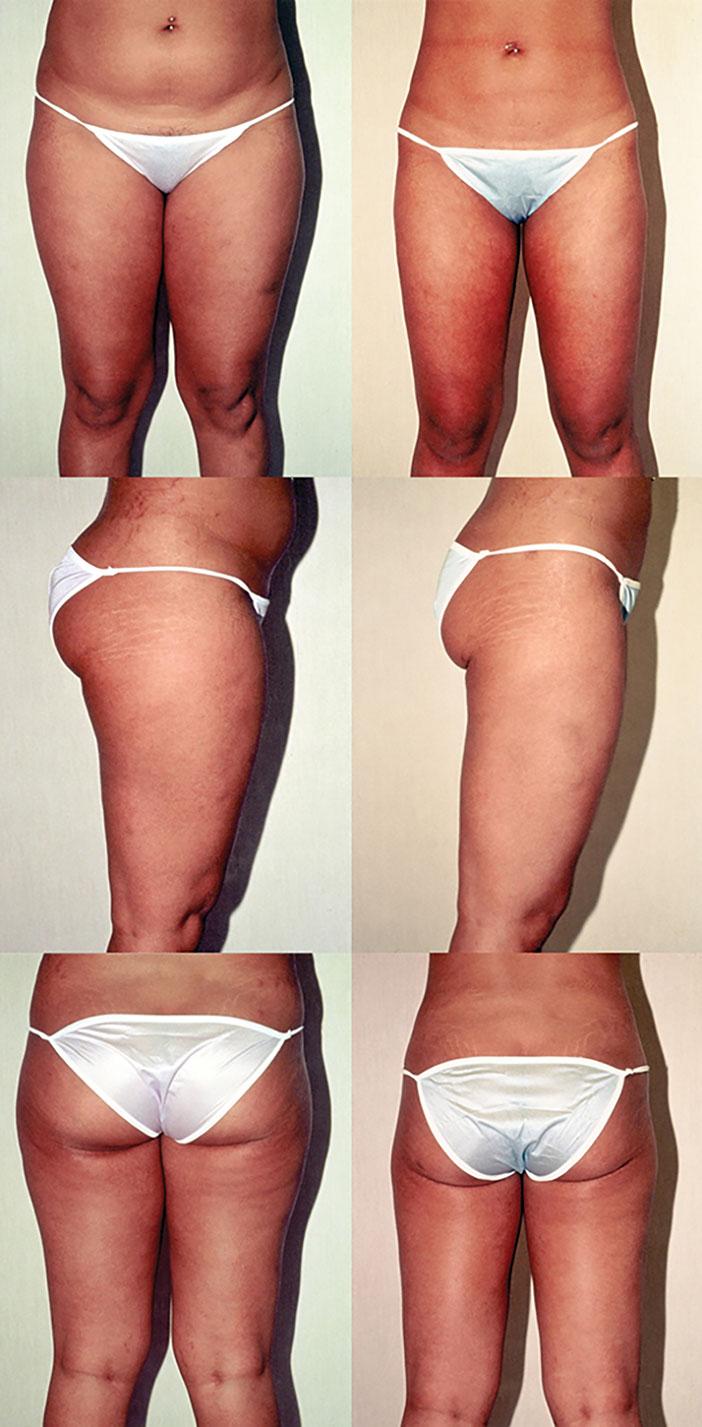
M.F., Age 39
Procedure: Liposuction of lower body
Before, 3 months after
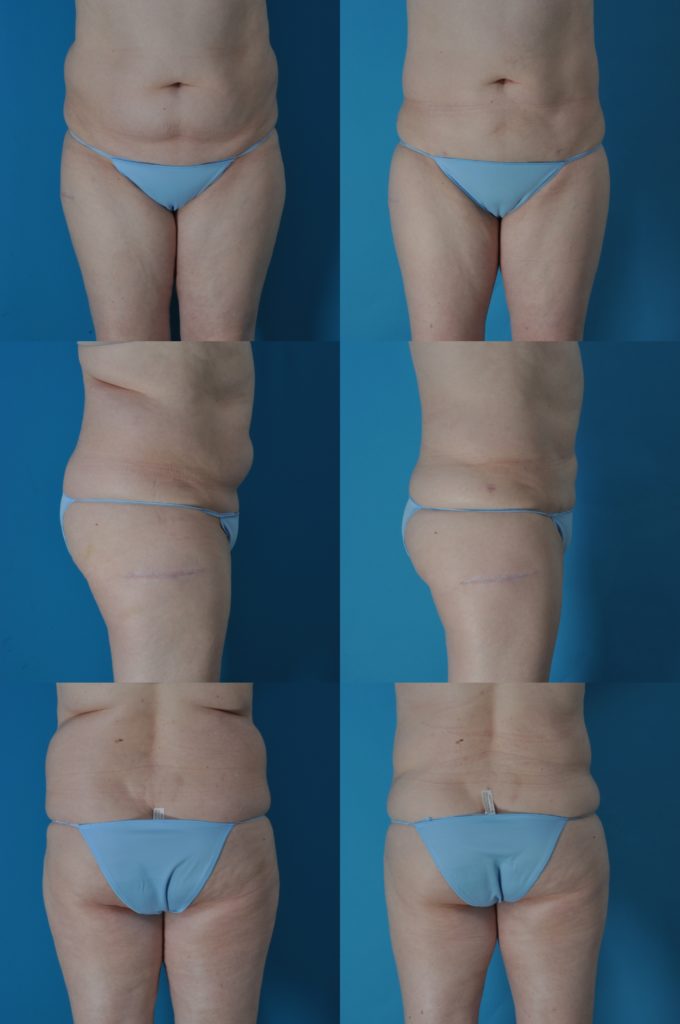
L.M., Age 39
Procedure: Liposuction of abdomen and flanks
Before, 4 months after
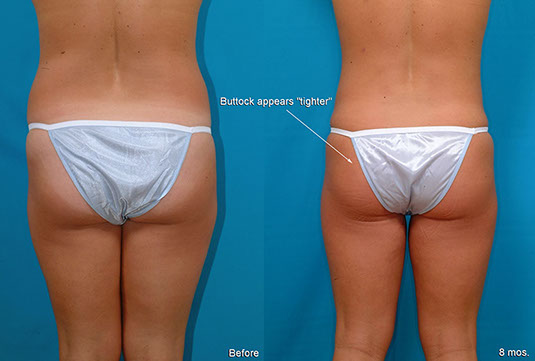
K.G., Age 49
Procedure: Liposuction of lower body, arms, and axillae, and submental lipectomy.
Before, 3 months after
M.M., Age 53
Liposuction of abdomen and flanks
3 months
A.S., Age 28
Procedure: Liposuction of lower body. Touch-up 11 months later: lower body.


Before, 1 year after
T.F., Age 26
Procedure: Liposuction of lower body, submental lipectomy. Touch-up 6 months later: abdomen, flanks, inner thighs and right posterior thigh.
Before, 11 months after (5 months after touch-up)
Liposuction with Breast Lift—Illusion of a Longer Torso
A.L., Age 32
Procedure: Liposuction of the abdomen, flanks, inner thighs and arms, breast lift, and breast implants. Touch-up 5 months later: abdomen, flanks, and inner thighs.
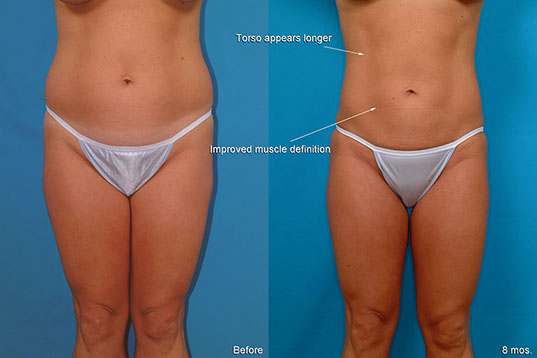

Before, 8 months after (3 months after touch-up)
K.M., Age 27
Procedure: Liposuction of lower body and breast augmentation. Touch-up abdomen, flanks, and thighs.



Before, 4 months after
B.D., Age 43
Procedure: Liposuction of lower body, arms and axillae, and breast augmentation.
Before, 16 months after
Pear-Shape, Long-Term Follow-Up
T.M., Age 34
Procedure: Liposuction of lower body, including calves and breast augmentation.
Before, 1½ years after, 8 years after
M.H., Age 54
Procedure: Liposuction of lower body, arms, and axillae.
Before, 3 months after
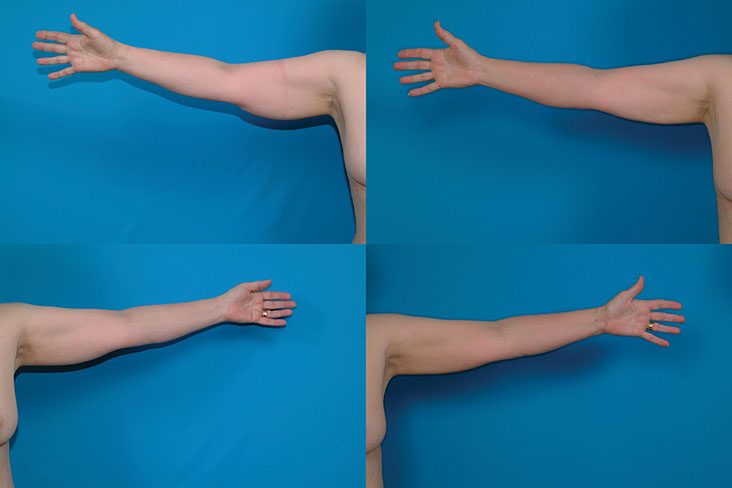
LIPOSUCTION OF ARMS
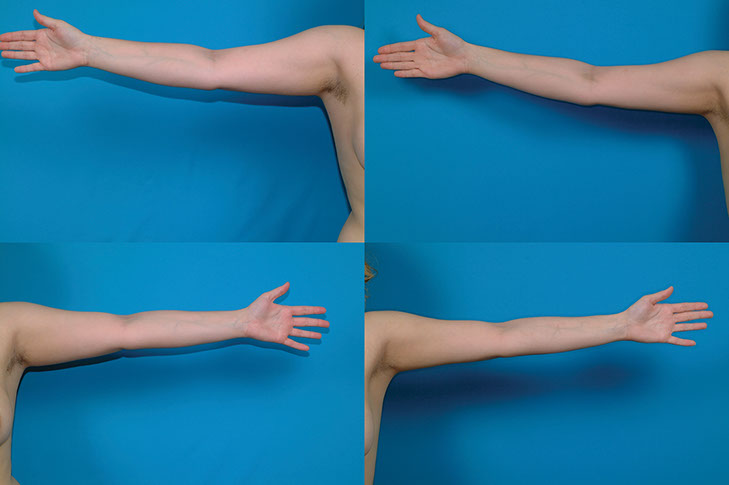
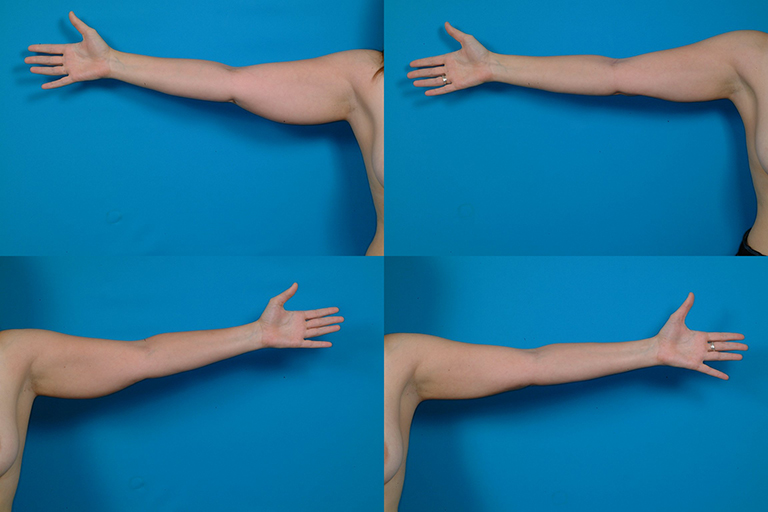
M.C., Age 22
Procedure: Liposuction of arms, flanks, inner thighs, and axillae, and submental lipectomy.
Before, 1 year after
D.H., Age 28
Liposuction of lower body, arms and axillae, and augmentation/mastopexy.
Before, 3 months after
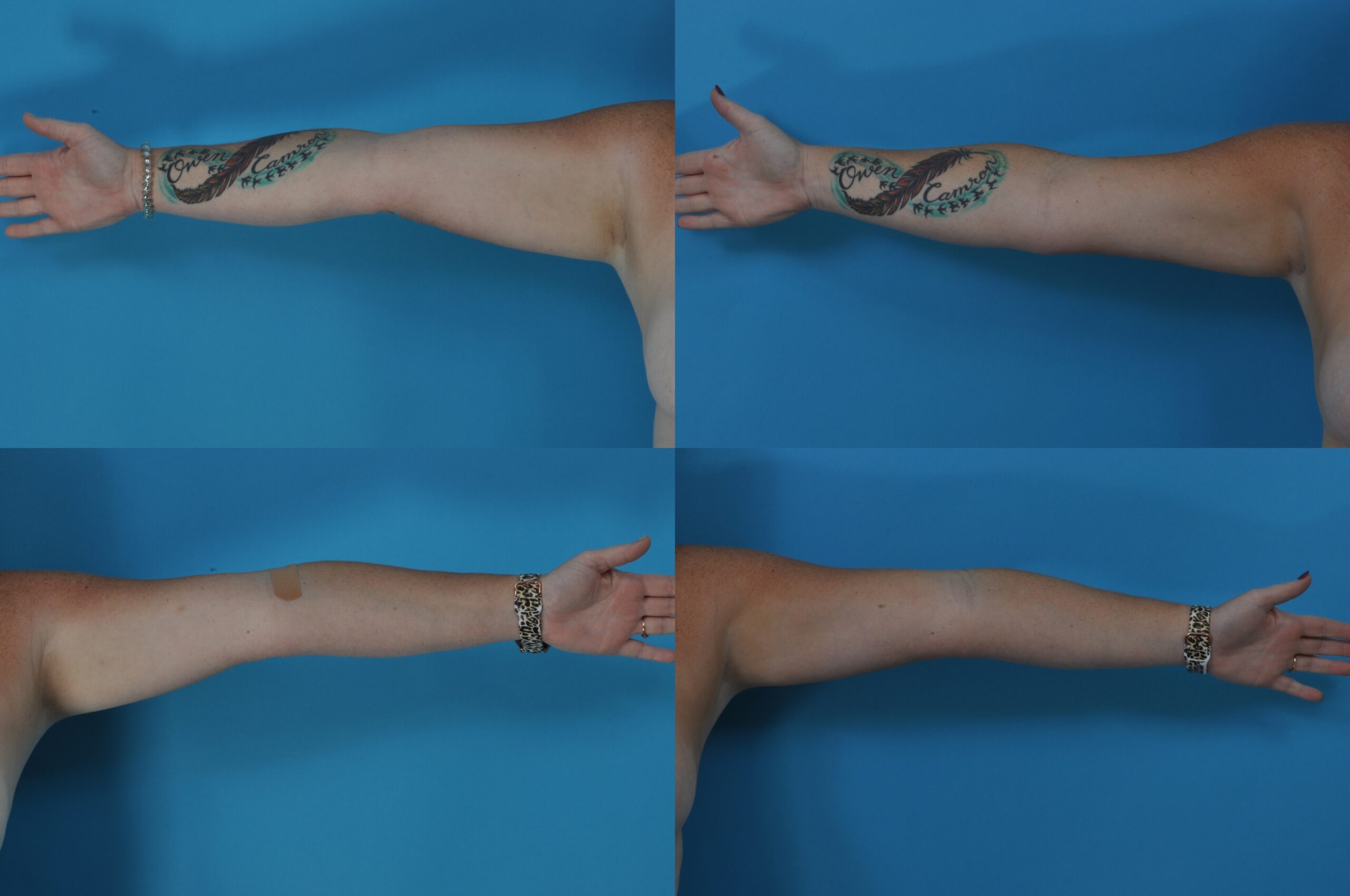
S.C., Age 32
Procedure: Liposuction of arms and axillae.
Before, 3 months after
K.M., Age 36
Procedure: Liposuction of abdomen, flanks, inner thighs, arms and axillae.
3 months
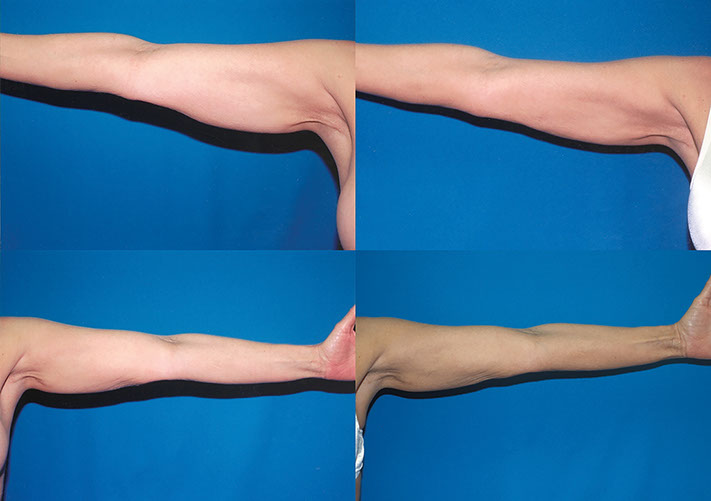
E.B., Age 39
Procedure: Liposuction of lower body, calves, arms and axillae. Touch-up 4 months later: lower body, arms, and axillae.
Before, 1 year after (8 months after touch-up)
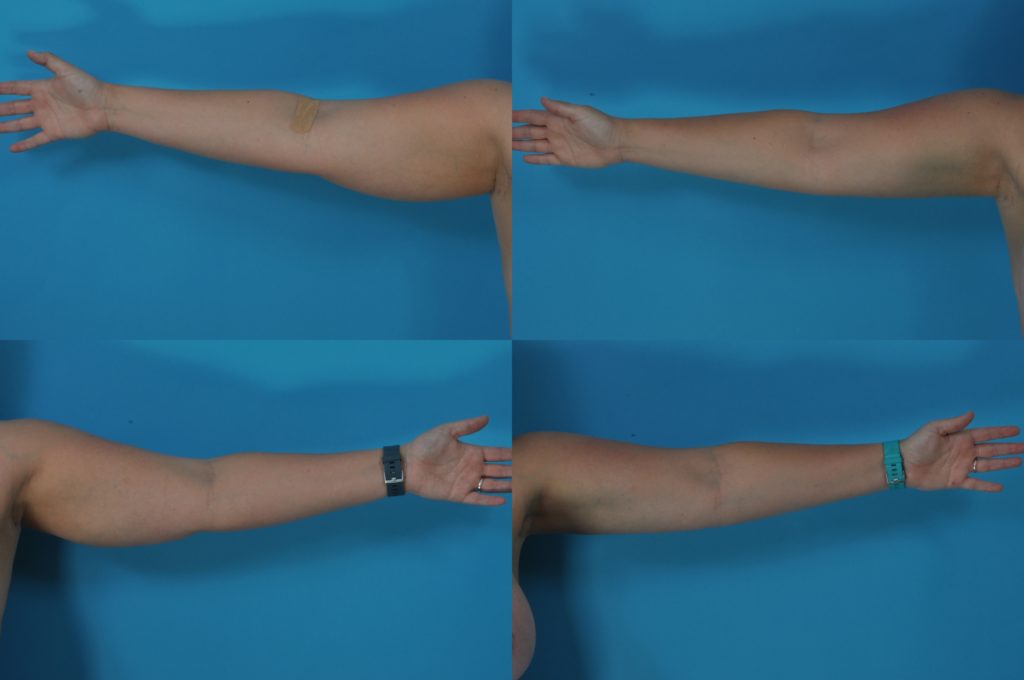
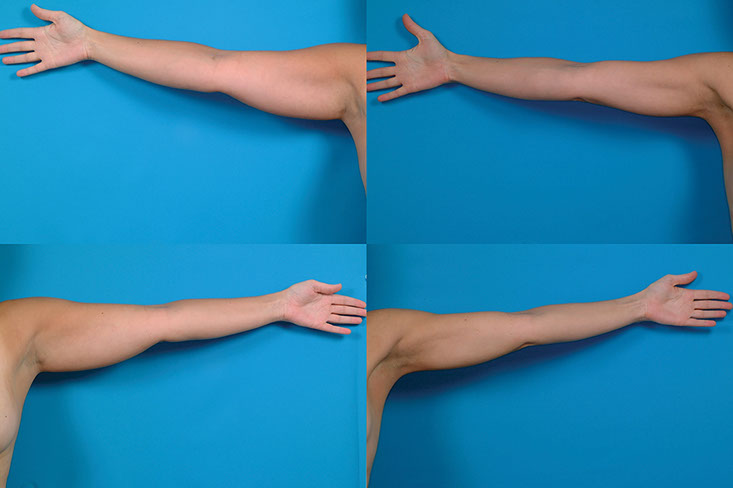
H.C., Age 42
Procedure: Liposuction of arms and axillae.
Before, 3 months after
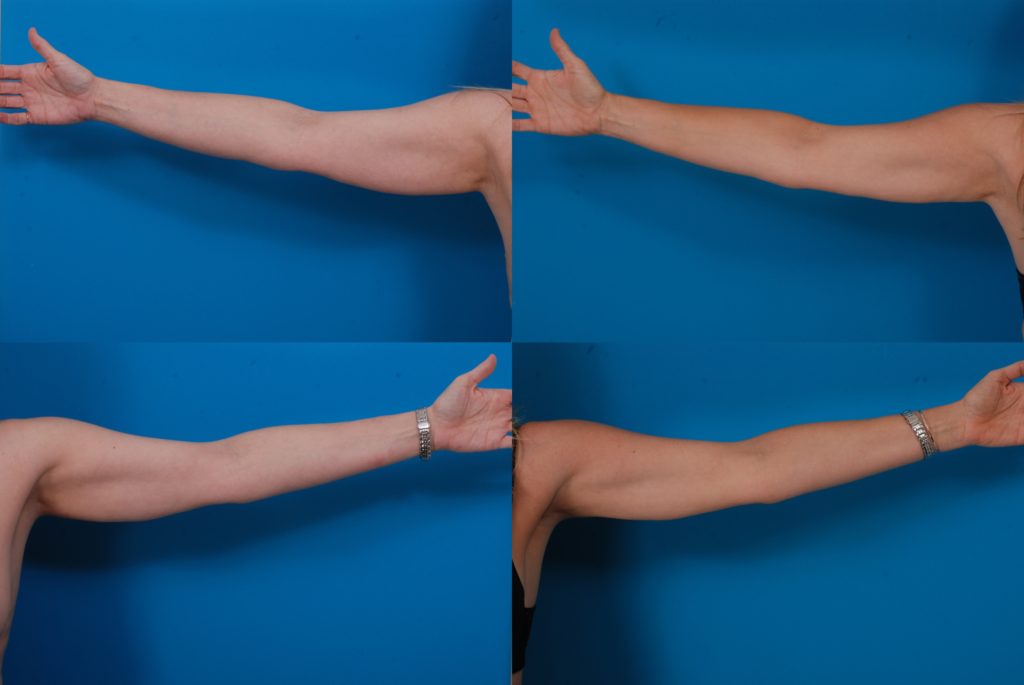
C.H., Age 58
Procedure: Liposuction of lower body, arms and axillae.
Before, 1 year after
L.B., Age 61
Procedure: Liposuction lower body and arms.
Before, 3 months after
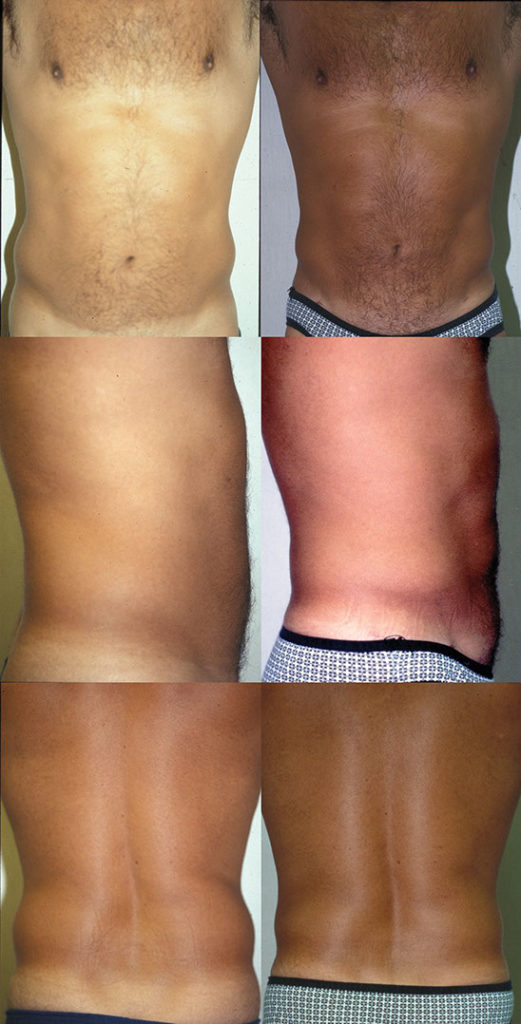
PHOTOS OF MALE PATIENTS
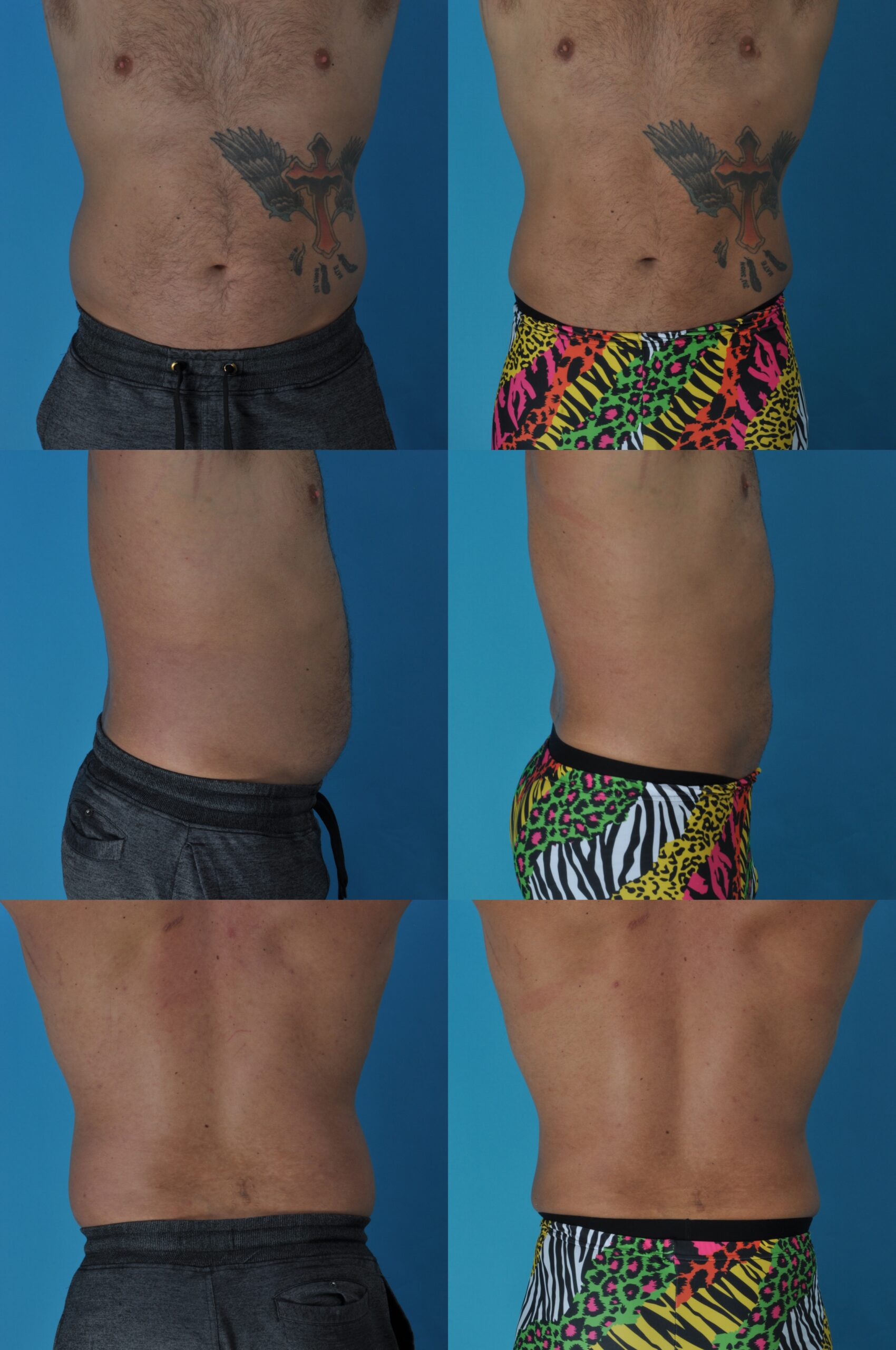
J.C., Age 39
Procedure: Liposuction of abdomen and flanks
Before, 6 weeks after
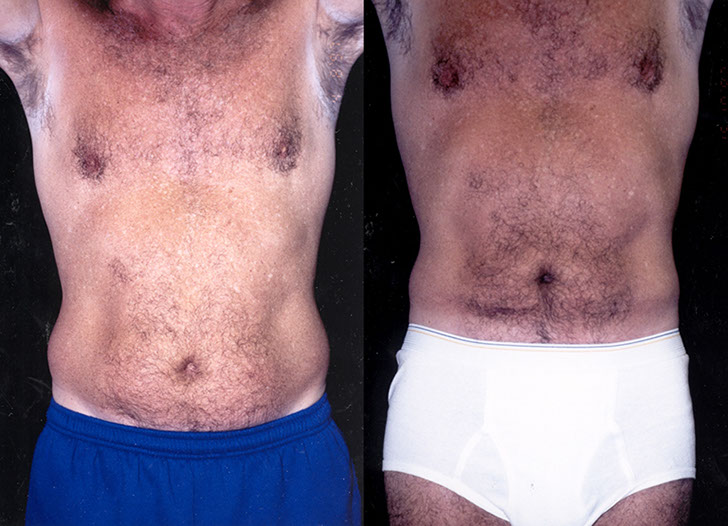
J.T., Age 45
Procedure: Liposuction of abdomen and flanks, and submental lipectomy.


Before, 6 months after
Liposuction After Weight Loss
D.D., Age 45
Procedure: Liposuction of abdomen and flanks
Before, 4 months after
L.M., Age 37
Procedure: Liposuction of abdomen, flanks, submental lipectomy and jawline augmentation.

Before, 6 months after
J.G., Age 40
Procedure: Liposuction of abdomen, flanks, breasts, and axillae and breast reduction
Before, 3 months after
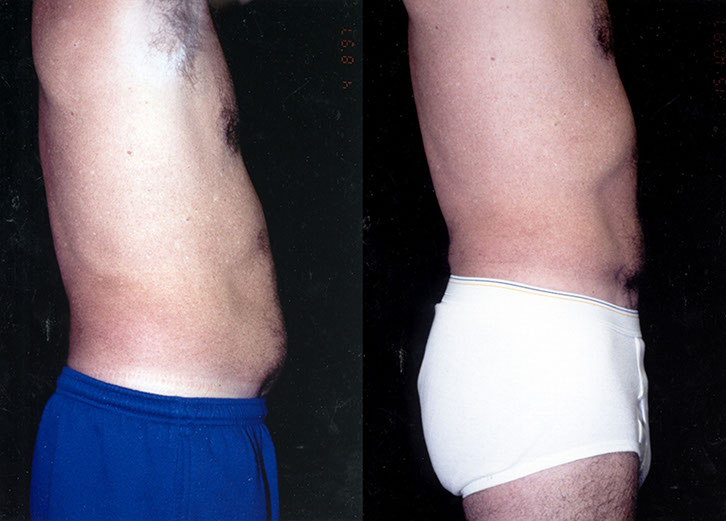
Men Over 50
K.H., Age 54
Procedure: Liposuction of abdomen and flanks

Before, 3 months after
J.S., Age 29
Procedure: Liposuction of abdomen and flanks (also direct excision of excess breast tissue) and
second liposuction 6 months later.
3 months after second liposuction
How It Is Done
Where Is It Done?
Today, body contouring surgery, including liposuction, is done primarily in ambulatory surgery centers and in-office operating suites. My patients have surgery at the Surgery Center of Leawood, an adjoining state-licensed ambulatory surgery center. All members of the American Society of Plastic Surgeons must use accredited facilities. This is an important safety consideration.
Anesthesia
Proper anesthesia is vital to patient safety. I prefer a total intravenous anesthetic. This is a form of anesthesia that provides, in my opinion, the ideal balance of patient comfort and safety. Patients are asleep for their surgery and wake up afterward with no recollection of the surgery. This type of general anesthesia differs from traditional general anesthesia in avoiding gas, intubation, paralysis, and mechanical ventilation. I call this type of anesthesia “SAFE” anesthesia. These letters stand for “Spontaneous breathing, Avoid gas, Face up, and Extremities mobile.” (Swanson E. The case against chemoprophylaxis for venous thromboembolism prevention and the rationale for SAFE anesthesia. Plast Reconstr Surg Glob Open 2014;2:e160.)
The surgery takes 1–2 hours, depending on the number of areas treated. Patients are asleep for surgery and awaken quickly afterward. Because local anesthetic is also used, patients require less medication and usually recover quickly after surgery, with minimal discomfort. Patients go home the same day.
How Do You Know How Much Fat to Remove?
The volume of fat removed is determined not so much by the surgeon as by the patient’s body characteristics and how much extra fat is present to start with. At first, the fat comes out readily, a stream of fat globules coming out the suction tubing that is gratifying to watch and listen to, as the fat globules reverberate down the suction tubing and spill into the canister. Gradually, the fat stream slows to a trickle. Also, the tissue resistance decreases. I keep a hand on the treated area and reassess the change in contour as the fat comes off. An experienced surgeon knows how far to “push the envelope.” This is the art of liposuction. It is important to take off as much excess fat as possible, to produce the best result for the patient, but it is even more important not to overdo the treatment. If the surgeon persists to try to take off another 10% or so, after the fat stream has been reduced to a trickle, this could cause unnecessary tissue trauma, more bruising, and increase the risk of skin irregularities or poor skin contraction. It is far better to avoid such problems, and return for a touch-up if necessary later on.
Most patients, right before surgery, tell me to take as much fat off as possible (“Don’t hold back, doc!”). Nothing personal, but they’d rather not come back for more surgery. Yes, they want it to be safe and all that, but they want as dramatic a result as possible!
I assure my patients that I will take off as much fat as I can without overdoing it and increasing the risk of complications. Patients understand that my job is to push the envelope as much as I can without pushing too far. I tell my patients I will treat them as if they are never coming back. The possibility of doing a touch-up later does not mean I’m going to leave to another time something I could do today.
A garment is worn to help reduce swelling for a period of 1 month. Patients wake up wearing it. This garment is removed for short periods to bathe and shower and may be worn under regular clothing. Bruising usually disappears within 1 month. Most of the swelling (about two-thirds) is gone in a month and patients may then wear shorts or a bathing suit. It takes about 3 months for the swelling to completely disappear.
The volume removed from each area is measured, in ccs. Often there is more fatty tissue on one side than the other so that it is common for volumes to be different from one side to the other. During surgery, I assess how much to remove visually, by looking at the treated area, using my hand to judge the level and pinch-test to assess thickness, feeling the tissue resistance, and by taking into account the volume removed, which the nurse records in real time as the fat is removed.
Liposuction and Anesthesia
Patients are usually aware of the importance of the anesthetic. Liposuction is unlikely to be a life-threatening procedure in itself. However, anesthetic factors such as airway management, fluid administration, and medication effects can be life-threatening. When I discuss complications, it is not unusual for me to discuss many of the details of how the anesthesia works, modifications that make it safer, and how patients are monitored during surgery.
Types of Anesthesia:
Local Anesthesia:
The area is numbed with anesthetic.
Many practitioners, particularly dermatologists, use local anesthesia exclusively. “Local” anesthetic is anesthetic medication that is injected directly into the tissues to numb them. The patient is awake during liposuction under local anesthetic. Advantages to the patient include the avoidance of a deeper level of anesthesia, less cost, and virtually no recovery time. A disadvantage is patient discomfort during longer procedures in which multiple areas are treated.
There was one memorable television report showing a patient casually talking on the telephone while having liposuction, but this is not the typical experience! Patients who have had previous liposuction elsewhere under local anesthetic typically tell me it was not a day at the beach and they welcome a short I.V. anesthetic.
Many surgeons, including myself, use local anesthesia alone only for small liposuction cases, such as a touch-up liposuction to limited areas. Patients tolerate this well and have minimal discomfort, like a trip to the dentist.
Conscious Sedation:
Patients are given intravenous medications to relax them plus local anesthetic. They remain awake during surgery. They may require substantial amounts of medication and can take several hours to fully recover after surgery.
General Endotracheal Anesthesia
The classical general anesthetic calls for a muscle relaxant, intubation, a breathing machine (“ventilator”), and an inhalational anesthetic agent (“gas”). Patients are paralyzed to allow mechanical ventilation, which necessitates an endotracheal tube to secure the airway.
This type of anesthesia certainly provides deep sedation, controlled ventilation, and a motionless patient for the surgeon. This level of anesthesia is necessary for major surgical procedures that require mechanical ventilation such as intra-abdominal surgery or open-heart surgery. But, it is a deeper level of anesthesia than is necessary for plastic surgical procedures, even for an abdominoplasty (tummy tuck).
There are additional risks related to general endotracheal anesthesia. Insertion of the endotracheal tube can occasionally be traumatic to the teeth and vocal cords. Positive pressure ventilation can overventilate patients, affecting their pH balance (respiratory alkalemia), causing secondary hypokalemia, and sometimes causing a pneumothorax. Anesthetic gas can cause nausea, irritate the bronchial linings, and may have a depressant effect on the heart muscle. Muscle relaxants paralyze the calf muscle pump, possibly increasing the risk of blood clots. Though rare, these agents can prolong the recovery time in patients with enzyme deficiency, trigger malignant hyperthermia (a potentially fatal complication), or allow unrecognized awakening in surgery. This is just a partial list of possible problems.
Total Intravenous Sedation
“SAFE” Anesthesia: Spontaneous breathing, Avoid gas, Face up, Extremities mobile.
This is the type of anesthesia that I use almost exclusively. The patient is asleep. The medications (propofol and fentanyl) are given intravenously. An LMA (short for “laryngeal mask airway”) is used during surgery to maintain the airway. Patients breathe spontaneously. They are not ventilated. They are not paralyzed and gas is not used. Patients are never turned prone (face down) during surgery. I consider this a “goldilocks” anesthetic—not too much (general endotracheal anesthesia) and not too little (local anesthesia or conscious sedation).
The anesthetist administers the medication through the I.V. tubing, and uses an infusion pump to provide a continuous delivery of a short-acting anesthetic called Diprivan (propofol). This “wonder drug” has made traditional general anesthesia unnecessary for many types of surgery, particularly outpatient surgery such as liposuction. Many patients are already familiar with this type of anesthetic, which has been used for years for G.I. procedures, knee arthroscopies and dental procedures.
If Diprivan is a “wonder drug,” the LMA is a “wonder airway”. Designed by a British anesthesiologist about 30 years ago, it provides a reliable airway without the need for intubation. This ingenious but weird-looking device lodges in the back of the throat and protects the airway, without going between the vocal cords. It is unnecessary for the anesthetist to intubate the patient. The LMA eliminates the need to pass a tube between the vocal cords, which can be difficult to do in some patients and occasionally traumatic to the vocal cords. Some patients still need to be intubated, such as those with esophageal regurgitation, but the majority may be safely treated with an LMA.
Once the patient is asleep, I inject dilute local anesthetic solution into all the areas that I plan to treat with liposuction. Why use local anesthetic if the patient is asleep already? There are two reasons:
- This way the anesthetist can use smaller amounts of propofol. The less anesthetic she gives, the less medication is in the patient’s system, and the faster the patient will wake up after surgery.
- The effect of the local anesthetic lasts for 8–10 hours, so there is minimal pain for the first several hours after surgery, making the recovery phase more comfortable, and reducing the need for painkillers after surgery. Less painkillers means less side effects from painkillers, such as nausea, sedation, and constipation.
As a general principle, any opportunity to eliminate a risk factor is worthwhile to keep the odds in favor of patient safety and comfort. This is part of the well-known “KISS” principle (Keep It Simple, Stupid). The incorporation of a technique that has a risk without a necessary benefit should be questioned. Rituals need to be examined. This is not easy for any surgeon who has developed habits.
Fluid Management
Using the tumescent technique, fluids are injected into the tissues before liposuction is performed. The original tumescent technique involved giving large amounts of fluid, as much as 10 liters, whereas the tissues became tightly distended. The “superwet” technique is a modified form of tumescent liposuction, in which fluids are infused in approximately a 1:1 ratio with what is suctioned off by liposuction (the “aspirate”). This represents an ideal relationship between what is infused and what is removed, providing a liquid medium to facilitate liposuction, but avoiding overhydration of the patient.
Positioning in Surgery
Prolonged motionlessness can cause problems. Nerves can be damaged by unrelieved pressure. Skin breakdown can occur at pressure points. It is advantageous to move patients during surgery. Our patients start supine on the operating table, but are then moved to one side and then the other when the anesthetic solution is injected. This turning routine is repeated when liposuction is performed. The patient is treated for about 30 minutes in a supine position, followed by 30 minutes on one side, and then 30 minutes on the other side. This ensures that there is no prolonged pressure while the patient is in one position. The intraoperative movement of the
lower extremities may also be helpful to avoid blood pooling in the calves (“venous stasis”) which can cause dreaded deep vein blood clots.
Many plastic surgeons place the patient prone on the operating table. This is the anesthetist’s least favorite position for some very good reasons. The airway is more difficult to manage and endotracheal intubation is needed. If the tube comes out, it’s a big problem because the patient is face-down. Pressure on the face is not ideal and can potentially cause problems. Pressure at the hips caused by rolls used to bolster the hips may interfere with venous return from the legs. There is often a period of inactivity, about 20 minutes, in the operating room while the patient is turned from face-up to face-down on the operating table. Often the patient needs to be re-prepped and draped because of loss of sterility.
Prone positioning is unnecessary. Moving the patient from side to side allows full-body access, avoids problems related to prone positioning, avoids a need for intubation, and improves operating time and efficiency by eliminating unnecessary interruptions.
The Incisions
I use as few incisions as possible to access the areas I need to treat. When treating the abdomen and flanks, I use an incision on either side of the pubic area and on each flank (see illustration). These are placed so that they would typically be hidden by a bikini. The access incisions for the thighs are in the groin crease on either side and on the lower buttock. The knee incision is tucked in the crease just below and on the medial (inner) side of the knee. These small scars fade with time and are usually inconspicuous. I do not use incisions placed midway along the arms, thighs, or calves, where they might be visible, or outside the bikini area on the abdomen and hips. The cannulae (long hollow instruments) are long enough to permit such limited incisions and still access all the areas.
Blood Clots (Deep Venous Thromboses)
The development of blood clots in the legs is a major concern. These clots can develop even without surgery. This is why flight attendants have passengers get up and move around on long flights. Inactivity raises the risk of blood pooling in the legs, called “stasis.” If a piece of this blood clot breaks off, it travels to the heart and then to the lungs, where it becomes a pulmonary embolus. This can be a fatal complication. Accordingly, it is important to take steps to minimize the risk of this complication.
Preventive measures include reducing periods of immobilization, such as very long surgery times or bed rest after surgery. It makes sense to avoid muscle relaxation, including the use of paralytic agents that are part of a traditional general anesthetic. Movement of the patient’s legs and position changes during surgery also make sense. Early ambulation is important. Getting up to go to the bathroom after surgery get the legs moving. Outpatient surgery forces the patient to ambulate during the first 24 hours. I usually see patients the day after surgery, so that I am assured they are up and moving. The trip to the doctor’s office helps. The objective is to reduce the risk of blood clots to a level as close as possible to the baseline risk that we have without surgery.
Blood Thinners
Some surgeons have recommended the use of blood thinners such as Heparin or Lovenox. Some newer types are taken by mouth—rivaroxaban (Xarelto) and apixaban (Eliquis). All of these medications can increase the risk of bleeding. It is impossible to accurately predict who will develop a blood clot, even by adding up potential risk factors. It is not clear that the increased risk of bleeding justifies the routine use of these medications (Swanson E. The case against chemoprophylaxis for venous thromboembolism prevention and the rationale for SAFE anesthesia. Plast Reconstr Surg Glob Open 2014;2:e160).
Ultrasound Surveillance for Blood Clots
The Swanson Center is presently engaged in a clinical trial to determine the feasibility and effectiveness of using Doppler ultrasound to screen patients before surgery, the day after surgery, and about 1 week after surgery. This highly accurate and noninvasive method can detect small clots before they grow and become dangerous. The results of ultrasound screening in 1000 consecutive plastic surgery outpatients were published in 2020. The findings were surprising in many ways. First, blood clots rarely formed during surgery. They were usually detected a week after surgery. Clots usually formed in the smaller distal veins of the legs and took about 5 weeks to resolve with treatment (oral anticoagulants). Sequential compression devices were of no clinical benefit. A simultaneous laboratory study showed no fibrinolytic benefit for these devices either. These results support total IV anesthesia and routine ultrasound screening This method can be used instead of “risk stratification” and “chemoprophylaxis,” which are questionable and can increase the risk of unnecessary postoperative bleeding.
1. Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96.
2. Swanson E. The effect of sequential compression devices on fibrinolysis in plastic surgery outpatients: A randomized trial. Plast Reconstr Surg. 2020;145:392–401.
3. Swanson E. Reconsidering the role of routine anticoagulation for venous thromboembolism (VTE) prevention in plastic surgery. Ann Plast Surg. 2020;85:97–99.
4. Swanson E. Distal deep vein thrombosis causing pulmonary embolism after outpatient plastic surgery: A case report. Plast Reconstr Surg Glob Open 2020;8:e2803.
5. Swanson E. Ultrasound surveillance offers a safe and effective method for venous thromboembolism prevention in plastic surgery patients. Aesthetic Plast Surg. 2020;231:783–784.
Outpatient Surgery
Improvements in anesthesia have shortened patient recovery times, allowing surgery to be performed safely in an outpatient setting. Benefits include greater convenience, easier scheduling, greater consistency in medical personnel, better cost-containment, and avoidance of hospital-acquired (“nosocomial”) infections. As a safety measure, the American Society of
Plastic Surgeons mandates that its members use only accredited outpatient facilities or licensed ambulatory surgery centers.
Liposuction of the Arms
The arms are a favorable area for liposuction. It is very common for me to treat the arms and armpits (“axillae”) at the same time as liposuction of the lower body. Women often complain about extra “flab” in their arms and will shake this area to demonstrate. They may be embarrassed about it and will avoid wearing sleeveless tops, even during the summer. Most women are understandably concerned about what will happen to the skin after the fat is suctioned. They don’t want to end up with a lot of loose skin hanging down. Often, the skin responds better than expected, even in older patients. The skin tone may be no better, but it is unlikely to be made worse and the removal of the extra fat improves the contour. It is always possible to come back and remove the extra skin (“brachioplasties”) if necessary.
However, I have had plenty of women over 50 with compromised skin tone who have had liposuction, and surprisingly few return for brachioplasties. It is always a plus to avoid a brachioplasty scar because this scar, which goes down the back border of the arm, cannot be completely hidden.
In patients who have lost a great deal of weight and have loose skin hanging to start with, it is better to proceed directly to brachioplasties, which are usually done in combination with liposuction. There is a limit, after all, to skin contraction. The brachioplasty scar is always preferable to loose skin that is sometimes called a “bat wing.”
“Bra Fat” (Axilla) Liposuction
Women often reach around and grab a roll of fat just lateral to their breasts. This is commonly called the “bra fat.” It can bulge around the bra strap, which is not very attractive. Even though this area is actually below the axilla, we refer to it as the “axilla” or sometimes the “scapular” area.
The same armpit incision used to treat the arms may be used for access to the axillary area. There is often a crease between this fat roll and the “love handle.” By treating the extra fat in the roll above and below this crease, the crease may be softened or sometimes eliminated.
Liposuction of the Arms: How It Is Done
An incision is made in the armpit. The area is first injected with anesthetic solution, the same way that liposuction is performed in other areas, using the “superwet” technique. The next step is removal of the fat using liposuction.
Some surgeons have been reluctant to treat the arms or calves because of concerns about complications. However, if the superwet technique is used, incisions are limited, and overtreatment avoided, these become very favorable areas to treat with minimal risk.
It is unusual for me to treat just the arms and axillae. Most women also have areas of the lower body to treat, so these areas are treated at the same time as liposuction of the lower body. The exception is the patient who has liposuction of the lower body and then returns to have the arms done. Of course, ideally these areas are treated in one operation. Because of the difference in fat distribution in men, very few men require liposuction of the arms, although I frequently treat the axillary areas when I perform liposuction on male breasts.
What To Expect After Surgery
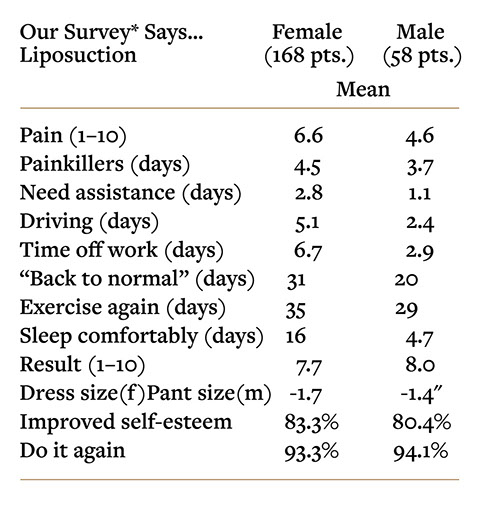
* Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129:965–978; discussion 979–980.
Discomfort
Local anesthetic is injected into the tissues as part of the tumescent (“superwet”) technique. This local anesthetic works for several hours, so patients are not in pain waking up after surgery.
If one leg is swelling conspicuously more than the other, this needs to be reported right away. Ultrasound scans are used to look for any blood clots that might be causing the swelling.
Survey results confirm that liposuction in males is less painful and the recovery is much faster than in females
(Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129:965–978; discussion 979–980.).
We all know this is not because men are more stoic than women (the conventional wisdom is the opposite). Women have more discomfort, on average simply because they typically have more areas treated and greater volumes removed. Women who have the abdomen and flanks treated alone (the areas most commonly treated in men), without the thighs, knees, axillary areas or arms, have recovery experiences similar to males. There is also considerable variability between individuals. The range of pain ratings was 1–10 for both sexes; some patients experienced virtually no pain and for others, it was the worst possible pain. Patient satisfaction was remarkably similar comparing men and women and the vast majority would have their surgery again.
Postoperative discomfort depends on the extent of liposuction needed and the number of areas treated. There is usually a generalized soreness and some stiffness due to swelling. Pain is typically well-controlled with medication, which is taken during the first several days after surgery. I have heard stories from patients who have been treated under local anesthetic, telling me how painful the procedure was. Some patients have friends who reported a lot of pain after liposuction. No doubt, liposuction can be a painful procedure. However, there are ways of reducing the pain. One way is by doing the surgery with the patient asleep, which is preferred for all but small touch-up liposuction procedures.
Local anesthetic is injected into the tissues as part of the tumescent (“superwet”) technique. This local anesthetic works for several hours, so patients are not in pain waking up after surgery. Also, tissue trauma is minimized using the ultrasonic technique, the less traumatic blunt cannulae, and avoiding overaggressive treatment. These precautions allow for superior results with tolerable pain levels. Most patients report that the pain level was what they thought it would be. It does not surprise them. It is tolerable and controlled by prescription painkillers.
There is still a range of patient experiences. Some patients take liposuction in stride, even returning to work the next day. Others give me a somewhat accusatory look (maybe I’m reading too much into it) and tell me, “I feel like I’ve been run over by a truck!” The number of areas treated is relevant. Most men have the abdomen and flanks treated, which is relatively easy to recover from. Some say it is like a tough workout in the gym. Most women also have the thighs treated. This causes more discomfort, particularly when sitting down.
Change in Clothing Size
Women dropped an average of 1.7 dress sizes (a drop from a 14 to a 10/12 would be 1.5 sizes). Men reported an average reduction of 1.4 inches around the waist.
A garment is worn to help reduce swelling for a period of 1 month. The garment is removed for short periods to bathe and shower and may be worn under regular clothing. Bruising usually disappears within 1 month. Patients may then wear shorts or a bathing suit. The stitches dissolve on their own.
Numbness
Numbness in the treated areas is to be expected. The small sensory nerve endings are traumatized by the surgery. There may also be unusually sensitive areas of the skin. This is called “hypersensitivity.” It typically takes about 2 months for the feeling to return to normal.
Swelling
Most patients notice a difference immediately after surgery. However, swelling develops during the first few days, which can make the areas temporarily look fuller than they were before surgery, particularly in lean patients. Accordingly, patients are instructed to wear loose-fitting clothing right after surgery. Although swelling is variable from patient to patient, typically two-thirds of the swelling is gone in 1 month. Full resolution of swelling takes about 3 months. This is important for patients to know, because they may otherwise be disappointed at their 1-month follow-up appointment, thinking that this is their final result, when in fact they still have a significant degree of swelling.
Many patients call the office several days or a week after surgery to report that their feet and ankles are swelling. They have a hard time putting on shoes. They wonder if this is normal. It is. The legs below the knees often show increased swelling a week after surgery because of the effects of gravity, even when the calves are not treated with liposuction. Bruising may extend all the way down to the toes. This may be alleviated by elevating your legs on an ottoman when you are sitting. If one leg is swelling conspicuously more than the other, this should be assessed by your surgeon because this could signal a blood clot in a leg vein (“deep venous thrombosis”), which is a serious complication requiring investigation and treatment.
The Garment
At the end of the operation, while patients are still asleep, a “compression garment” is applied. This is either a simple Velcro binder that goes around the abdomen and flanks (commonly used in men), or a girdle that goes from the level of the upper abdomen down to the thighs, either above or, more commonly, just below, the knees. The purpose of the garment is not to even out the fat layer. The remaining fat cells do not move around, which is why technical expertise in evenly removing the fat cells is important. The garment is not used to smooth contours. Rather, it is used to limit swelling, and help the swelling to go down sooner. Most patients also find it more comfortable to wear the garment. They feel that they need the support. It is removed for bathing, and may be washed, although it should be dried in a no-heat cycle to avoid shrinking. It is difficult for women to put on the girdle at first; they need help. But after changing it a few times, it becomes easier. One trick is to leave the bottom end of the garment at the knees zipped for several inches so that it does not become tangled when it goes in the wash.
I usually recommend wearing the garment for 1 month. It is concealed under clothing, except during the summer when Capri pants may be necessary to conceal the knee-length girdle (when the knees are treated). However, 2 weeks after surgery, patients may wear spandex instead, such as cycling shorts or an aerobics outfit. You can alternate wearing the garment and wearing spandex. The principle is gentle compression. Some patients are never comfortable with the garment and make the switch to spandex earlier. It is important to realize that too loose is better than too tight. If you don’t wear the garment at all, your result will be the same, but your swelling will take longer to go down. I recommend wearing slightly compressive athletic garments when exercising, even after a month. This helps reduce swelling.
Time Off Work
Time off work depends on the areas treated, how physical requirements of the job, and your own pain tolerance. Most women take 1 week off work, or 2 weeks if they have a job that requires significant physical activity. Men usually recover quickly because fewer areas are treated and are often back to an office job in 3 or 4 days. Some return to work the day after surgery. For more physical jobs, such as a plumber or construction worker, 1 week off is recommended. If the job is very physical, such as going up and down ladders, 2 weeks off is better. For women, who usually have the lower body treated (thighs included), 1 week off is recommended for office jobs. However, plenty of my patients return to work sooner. If you have a job that involves standing for long periods (pharmacist, for example), a week off is recommended. Otherwise, you will swell more and be uncomfortable at the end of the day. Sitting is uncomfortable after having the thighs treated and you will want to get up frequently and move around.
Exercising
Most patients want to know when they can get back to exercising. Many work out on a regular basis, some every day. The most difficult aspect of the surgery may be interruption of their exercise routine. I tell them, no exercising for 2 weeks, and they give me the look that says, “maybe for other patients, doctor, but not me.” I then explain that they will be sore after surgery and if they do work out, they will have more swelling and will hurt more afterward (not while they are working out, but later). It is possible to get some nonvigorous exercise, by walking for example, but any vigorous exercising that raises the blood pressure will exacerbate swelling. Using an elliptical trainer or exercise bike should wait about 3 weeks after surgery. All exercises may be resumed 4 weeks after surgery. When resuming exercise, it is important to let your body tell you when you are ready. First do a light workout, maybe 50% of what you would ordinarily do, and then see how you feel the evening after exercising. If there is no problem, increase your exercise routine gradually. If you do it all at once, you will swell and hurt more, and will need to take more time off before resuming exercising, but fortunately, this will not jeopardize your result.
Back to Normal
Another common question is, “When can I go on a cruise?” I’ve had patients go on Caribbean holidays days after surgery, but most people want to look and feel their best. One month after surgery, the bruising and most of the swelling is gone. There are no restrictions at this point, so a minimum of 1 month of recovery time is recommended.
Liposuction of Arms
There is no garment that is applied to the arms. However, some patients will wear a snug athletic shirt that has sleeves to provide some gentle compression. Swelling and bruising are to be expected. The bruising may extend down the forearm due to gravity. There are areas of numbness that can take a few months to return to normal. The arms are sore, but the pain is tolerable. Often a caretaker may grab the arm to help, not realizing that it is sore. Because the arm is at a higher level than the heart, arm swelling tends to go down more quickly after liposuction than the legs. Liposuction of the arms does not seem to add much to the amount of postoperative discomfort, and improves an area that is more visible and responds favorably, so it is common for women to have the arms treated simultaneously with their lower body.
Complications
Skin Excess
Liposuction is primarily a procedure to remove excess fat. It does not remove extra skin. Patients who have extra skin causing rolls in the abdomen are usually better served with a tummy tuck (“abdominoplasty”) simultaneously with liposuction. However, there are areas where the scars from a skin excisional procedure are more obvious, such as the arms and inner thighs. Here, we often do liposuction even in the presence of loose skin, hoping that a modest degree of skin contraction will help. It is possible to come back later and remove extra skin if necessary. However, it may be best to accept some skin looseness and avoid a scar.
Cellulite
Although liposuction is a good technique to remove extra fat cells and improve proportions, it is not consistently helpful for treating cellulite. In fact, there is no treatment available today that is good for treating cellulite, despite claims to the contrary and machines that are marketed and “FDA approved” for this purpose. Patients are disappointed to hear this news. Cellulite is a big, unsolved problem. In some patients, it may be possible to achieve modest improvement but patients should not count on this.
Fortunately, liposuction does not usually make cellulite worse, except for situations of poor skin laxity, where an excisional procedure such as a tummy tuck or thigh lift may be appropriate. The type of cellulite that is improved by pulling up on the skin (“secondary” cellulite) can be improved with a lifting technique such as a thigh/buttock lift, but this is a major procedure and does involve a long scar along the hip line. A thigh/buttock lift (when combined with a tummy tuck, this is called a “lower body lift”) is typically recommended for patients after major weight loss, or in patients whose cellulite is so severe that it prevents them from wearing shorts in the summer.
Asymmetry
During surgery, measurements of the amount of fluid injected and the volume removed (“aspirate volume”) are recorded. This helps to ensure symmetrical treatment. Of course, asymmetrical fat distribution is common, so it is not unusual to take more volume out from one side than the other.
Seroma (Fluid Collection)
If excessive tissue trauma avoided, seromas are rare. They tend to occur more frequently in areas that are simultaneously undermined, creating a pocket in which fluid may accumulate, such as under the chin after a submental lipectomy, or abdomen after an abdominoplasty.
Overtreatment
Overtreatment is much more difficult to treat than under-treatment. It is not difficult to return to do more liposuction. However, if too much fat is removed, restoring normal contours is a challenge. Fortunately, fat injection is available and can be used to fill in defects.
Bowel Perforation
Patients occasionally ask about the risk of puncturing an organ during liposuction. The most important safety consideration is the surgeon’s experience. The cannula is passed horizontally in the subcutaneous plane, where there is minimal resistance. It is usually not difficult to stay in this plane. The use of the “superwet” technique, and blunt cannulae help. Previous surgery which may cause scarring of this plane or hernias may increase the risk. Ultrasound scans are routinely done to check for hidden hernias.
Care After Treatment
Getting Back to Normal
Drainage from the incisions is normal during the first 24–48 hours. This may cause blood-staining of the garment.
You can shower and bathe after your appointment the day after surgery.
When getting ready to shower, remove the garment and then sit down for several minutes before getting up. This gives your body a few minutes to adjust because your blood pressure will drop a little with the garment off. When you are up, if you feel light-headed, immediately lie down and this will correct itself. After a few days, this does not seem to be a problem anymore.
You will probably need some help taking off the garment and putting it back on during the first few days. Then you will get the knack of doing it yourself.
Swelling and bruising are to be expected. Keep in mind the bruising is affected by gravity. Areas such as the flanks and the back of the thighs tend to bruise more because you sleep on your back. If your thighs are treated, the swelling and bruising can go down your legs, even to your ankles and feet. Usually, when the abdomen is treated, there is swelling and bruising of the pubic area, often going down to involve the genitalia. Don’t worry about bruising and swelling of this area, it is normal.
Wear the garment day and night. Take it off to bathe and wash the garment at the same time. Wash the garment in a gentle cycle in cold water and line dry or place it on the air-fluff dryer setting.
After 2 weeks, you can alternate and wear spandex for periods of the day, which is likely to be more comfortable. Aerobic outfits or cycling shorts usually contain this material, which provides compression. The principle is even compression of the treated areas for comfort and to reduce swelling. You should wear the garment for a month.
The Band-Aids can come off after 2 days, or sooner if they are saturated. Leave the Steri-Strips on another couple of days (don’t worry if it comes off with the Band-Aid). Usually, you don’t need to apply another Band-Aid unless there is still some drainage or the incision is in an area that might be subject to friction from the garment. The sutures dissolve on their own.
Contact the office if you are having excessive fainting, nausea, swelling, pain, or fever over 101.0°F or 39.5°C. Swelling of the feet and ankles is normal if you had your thighs and knees treated. But, if the swelling seems to be much greater on one side than the other, this may signal a blood clot and you need to come in to have this assessed.
The bruising can take up to a month to go away. Swelling takes longer. About 80% of the swelling is gone in a month and virtually all of it is gone in 3 months. This is the reason why we usually take photographs 3 months or more after liposuction.
FAQ’s
Q: Does it hurt?
A: The pain level is moderate and usually well tolerated. Patients tell me it is about what they expected.
Q: Does the fat come back?
A: The fat cells removed by liposuction are gone forever. Fat cells that are left behind can swell if you gain weight and shrink if you lose weight, but the numbers are reduced forever. Liposuction offers a permanent improvement in body proportions.
Q: Where do you make the incisions?
A: I use as few incisions as possible to cover the areas I need to treat. When treating the abdomen and flanks, one incision is made on either side of the pubic area and one is made on each flank. These are placed so that they would typically be hidden by a bikini. The access incisions for the inner thighs are in the groin crease on each side. The outer thighs are accessed using the same incisions used to treat the flanks, and through an incision on the lower buttock. The knee incision is tucked in the crease just below and on the medial side of the knee. The small scars fade with time and are usually inconspicuous. If any are found objectionable, they may be revised.
Q: Do you leave the incisions open?
A: No. Some patients have heard that the incisions are left open to allow fluid to drain out. However, most plastic surgeons prefer to close them and allow any remaining fluid on the inside to be absorbed. This makes it easier for the patient because it is not as messy afterward. Also, the incisions heal better and with less scarring if they are sutured, as opposed to leaving them to heal in on their own.
Q: Do I have to wear a girdle?
A: It sounds onerous, but most patients feel more comfortable in the garment after surgery. The garment helps limit swelling. You will need to wear it for a month after surgery.
Q: Will liposuction help my cellulite?
A: You should not expect much improvement in cellulite. Liposuction removes fat and improves proportions but is not primarily for smoothing skin irregularities. We still do not have a good treatment for cellulite. I certainly have had patients whose cellulite is improved after liposuction, but I am careful not to promote liposuction as a cellulite treatment. It is a body shaping treatment. If a patient has an improvement, it is welcomed, but it should not be expected.
Q: What about CoolSculpting?
A: Results are unimpressive and may not be worth the time and expense on the part of patients. It has many limitations. Liposuction is the only treatment that can provide comprehensive and continuous contouring involving all areas of the body. For the patient who wants results, there is no substitute for liposuction when performed by a skilled, experienced surgeon. Not surprisingly, liposuction continues to be the most popular cosmetic surgical procedure performed today.