INTRODUCTION
How Do I know If I Need a Breast Lift?
Women’s breasts sag as they get older due to gravity, pregnancies, hormonal changes after menopause, or after substantial weight loss (over 50 pounds). Heredity is also a factor. Women are often aware of other female family members who are similarly affected.
Sagging never gets better with age, and does not respond at all to exercise, wearing a bra all the time, or any lotions that are applied to the skin.
Women with troublesome sagging who wish to correct it may benefit from a breast lift (“mastopexy”), which may often be conveniently performed at the same time as an augmentation.
When is sagging troublesome? Here are some clues:
- When sagging is the main complaint about the appearance of her breasts.
- When we both agree that her sagging is beyond borderline.
- When she looks at photos showing the minimal degree of sagging improved by augmentation alone and finds it is not enough.
- When she looks at the photographs of results and scars from a breast lift and finds the trade-off acceptable.
- When we both believe she may have regrets and return for a lift later if she does not have it at the time of her augmentation, and she would prefer not to have a second operation.
- When she does not want to be larger, just lifted.
- When she desires smaller areolae anyway.
- When her nipples are down-pointing.
Breast Implants to Restore Fullness—Still the Gold Standard
Women who have borderline breast sagging may be best treated with implants alone, which improve fullness. Breast implants reliably increase breast projection and upper pole fullness. The nipple is not changed in relation to the surrounding skin, but the increased volume of the breast causes the nipple to project farther. A breast augmentation may be the right choice for the younger patient who can accept a mild, natural degree of sagging if this means she can avoid the extra scarring that comes with a breast lift. Of course, she can always wait and have a breast lift in the future. It is also the right operation for an older woman (over 40) who wants to look good in her bra but is not too concerned if the nipple position is still low. She’ll tell me, “I’m not trying to be 20 again.”
Most patients, however, do want to correct the sagging and do not wish to have their nipples riding low on their breasts.
I find that younger women (20s and 30s) will generally opt for a breast augmentation, and older women (40s and older) more readily accept a breast lift. However, I certainly have operated on plenty of women in their 30s who have elected to have a lift with their augmentation, particularly if their nipples are already starting to point down. They recognize that the problem is not going to improve and they are going to have a lift at some point anyway, so why not do it now? It is also true that younger women will generally prefer larger breasts than forty and fifty-somethings. Of course, larger breasts can give the illusion of being heavier, and older women prefer the svelte look, undoubtedly because it is harder to achieve as we age. They do not wish to appear matronly.
Breast Augmentation vs. Breast Lift
For women whose primary concern is breast sagging, or downward drift of the nipples, a breast augmentation and lift (augmentation/mastopexy) is the right combination. These women are basically fed up with their breast sagging. They tell me that they don’t feel comfortable in bathing suits or dresses or that they feel sloppy and this makes them self-conscious. It affects their self-esteem. These women are often less concerned by scarring if this procedure can give them the lift they want.
If a woman lifts her breasts up in the cups of her hands and says “This is what I want,” the operation of choice is breast lift and implants (“augmentation/mastopexy”).
The downside of a breast lift is more scarring and this must be weighed against the improvement in shape. For patients who simply wish to fill out their bra, or if they do not wish to have the breast lift scars, I recommend implants alone. The patient may always return at a later date for a breast lift.
If correction of sagging is a priority, then a breast lift is recommended. Breast augmentation alone will not suffice. For women who wish to wear clothing that does not rely on a bra, such as bikinis, halter tops, or dresses with spaghetti straps, a breast lift is recommended.
If a patient reacts negatively to the scars on viewing before and after photographs I show her in my office, a breast lift is obviously not for her. If there is any hesitation about the scars I tell women to wait. There will be a time later on when they will look at the scars, look at the shape, and say: “When can we do it?” With this approach, my breast lift patients are among my happiest. Patients would not trade their scars for sagging breasts, even if their scars are not ideal. They find their scars are hidden in most bathing suits and evening gowns.
Breast augmentation alone provides minimal improvement in sagging. One would think that a breast implant would take up the slack in the breast and provide the desired elevation, but the amount of breast lift is minimal (0.6 cm), compared with 5 cm for a breast lift and 4 cm for the combined implant/lift. Usually, the nipple level stays about the same after an augmentation alone. The crease under the breast (“inframammary fold”) actually lowers after implants (Swanson E. Photometric evaluation of inframammary crease level after cosmetic breast surgery. Aesthetic Surg J. 2010;30:832–837.). Many women, and even plastic surgeons, believe that the nipple will ride up once implants are inserted, but measurements show this is not the case. If low-set nipples are a concern, there is no substitute for a breast lift, which is very effective at elevating the nipples. The average lift in nipple position after a breast lift is almost 6 cm (4.5 cm for the combined procedure), compared with only 0.3 cm after implants alone. (Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/mastopexy, and breast reduction. Plast Reconstr Surg. 2013;131:802e–819e.).
The Benefits of a Breast Lift
- A lot of improvement in sagging.
- Nipple elevation.
- Better shape with more projection and upper fullness with the newer vertical mastopexy technique.
- The vertical mastopexy procedure eliminates the long horizontal scar that was part of the older, inverted-T “anchor” procedure.
- Many women welcome smaller areola, an extra benefit of a breast lift, which makes use of an incision around the areola. Women with large breasts tend to have larger areolae, and about half find them too large. This is because the same process that stretches out the breast also stretches out the areola.
- The illusion of a longer torso.
Many women regard the reduction of areolar size as an acceptable trade-off for a scar that goes around the areola. There is a scar around the areola and a vertical scar, which form the “lollipop” scar. By avoiding the long horizontal “anchor” scar (a shorter scar may still be used in the inframammary crease to avoid a scar continuing on to the abdomen) used in the past, the trade-off (improved shape vs. scars) is much more favorable today for women having a breast lift. The decision to have a breast lift is an important one. But there are enough clues that it is unusual for the patient and I not to come to a consensus after talking about these issues and looking at photographs. Women often wonder what their husbands or boyfriends will think of the scars. The easiest way to handle this is for the significant other to be there at the time of consultation and also review photos showing the scars. In my experience, feedback from male partners has been very positive. But, the bar I set is high. In the patients I treat, the trade-off has to be strongly in favor of the lift. Women with mild sagging are probably best to accept the sagging rather than commit to the scarring that comes with a lift.
In severe cases of sagging, the nipples may be located at the lowest part of the breast, pointing down. Women with downward pointing nipples find their breasts unattractive and understandably wish to have their nipple lifted up where they are supposed to be. Women may find that they have a positive “pencil test”—they can hold a pencil under their breasts without using their hands. In this case, “positive” is not good. One patient of mine joked that she could pass a “bar of soap” test too!
Does Wearing a Bra Prevent Sagging?
Women sometimes ask me if wearing bras helps prevent sagging. To my knowledge, there has never been a study done to assess this, but certainly wearing bras does not prevent it—American women by and large wear bras and still develop sagging.
Degrees of Sagging
Traditionally, when plastic surgeons have discussed breast sagging, they have referred to the position of the nipple in relation to the crease under the breast (inframammary crease or inframammary fold), the Regnault classification. In youthful, attractive breasts, the nipple sits at about the same level or above this crease. With progressive breast sagging, the nipple typically drops below the level of this crease as it descends with the breast.
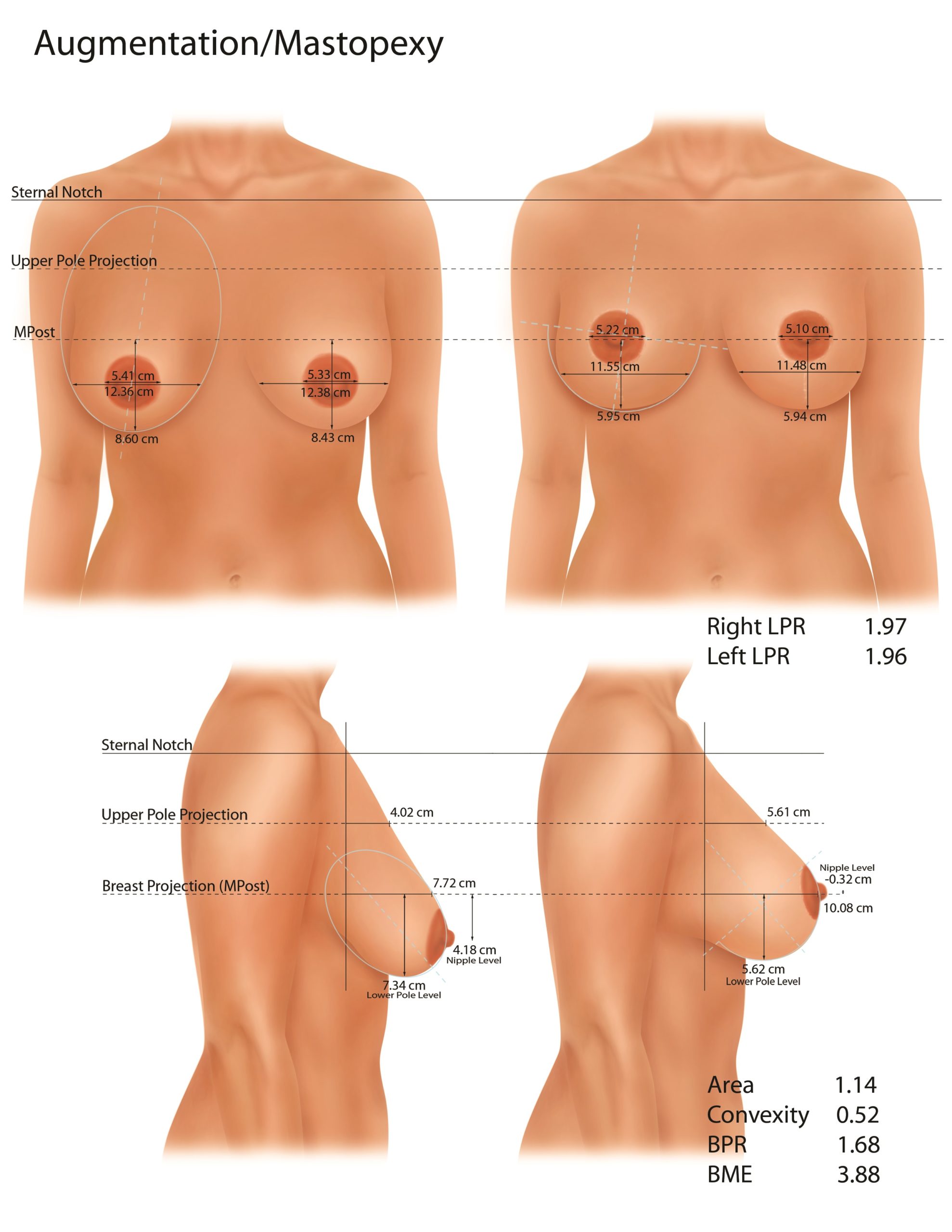
A New Breast Measurement System
A limitation of the Regnault classification is that it relates the nipple position to the level of the inframammary crease—which can change after surgery—rather than to the breast. This system is one-dimensional, and cannot describe breast shape. Three-dimensional methods have been used, but are complicated. Until recently, breast projection and upper pole fullness had not been precisely defined. To remedy this deficiency in our measurement capabilities, I developed a new breast measuring system (Swanson E. A measurement system for evaluation of shape changes and proportions after cosmetic breast surgery. Plast Reconstr Surg. 2012;129:982–992; discussion 993) based on a reference plane—the plane of maximum postoperative breast projection (MPost). This system provides a means to measure breast projection and upper pole projection, two desirable characteristics. This reference plane is also used to determine the “breast parenchymal ratio”—the ratio of breast area above and below this plane. The preferred ratio is about 1.5:1. Women with sagging breasts often have a ratio of 0.8. Women prefer more fullness of the upper breast than the lower breast, which is not surprising in view of the purpose of bras.
Another measurement, the “lower pole ratio,” assesses the tightness of the lower pole. A semicircle has a ratio of 1.73. Lower pole ratios over 2.0 start to appear boxy. The inverted-T techniques were prone to creating boxy breasts because of the geometry of the procedure, which trades breast projection for width, the reverse of what is needed (Swanson E. Comparison of vertical and inverted-T mammaplasties using photographic measurements. Plast Reconstr Surg Glob Open 2013;1:e89). The vertical breast lift procedure does just the opposite, trading breast width for projection. The geometric effect is favorable—more projection and a tighter, more conical, lower pole.
Saggy and Too Large
Mae West was not talking about breasts when she said, “Too much of a good thing is wonderful.” Over-endowed women have just as much trouble as under-endowed women, or more, because there may be physical problems in addition to the psychological ones. There is an operation for every degree of breast sagging and size. It is possible to reduce the breast size slightly by taking out a small amount of breast tissue with the skin, or dramatically reduce breast size (at which point it is called a breast reduction), by removing skin and a lot of breast tissue. Insurance companies often use 500 grams as their benchmark for deciding when a breast lift amounts to a breast reduction. They don’t want to pay for breast lifts, which they consider cosmetic.
Interestingly, our study found that not only breast reduction patients, but also women with less than 300 grams of tissue removed per breast (normally considered “breast lift” patients) report significantly reduced symptoms of neck, shoulder, and back pain after surgery. The finding that women who had smaller resection weights also had relief of symptoms shows that the distinction between a breast lift, typically considered a cosmetic procedure, and a breast reduction, traditionally done for symptomatic relief, is artificial. A breast lift can be considered a small reduction and these patients can feel better in addition to looking better. (Swanson E. Prospective outcome study of 106 cases of vertical mastopexy, augmentation/mastopexy, and breast reduction. J Plast Reconstr Aesthet Surg. 2013;66:937–94)
Both procedures—breast lift and reduction—have functional and aesthetic benefits. The incisions for a breast lift and reduction are the same if the preferred vertical method is used. The only difference is the weight of breast tissue removed, and whatever weight standard is used to separate the two is arbitrary (I use 300 grams).
Saggy and Too Small
Many women have breasts that have gotten saggy and lost volume too. This typically happens after pregnancy. For these women, the sagging may be treated with a lift, and the breasts are simultaneously enlarged with implants: a breast lift and augmentation. Plastic surgeons call this operation “augmentation/mastopexy.”
Women need to know that a breast lift alone will not give them more fullness in the upper poles. You might think that the plastic surgeon could simply push the existing breast tissue up, filling out the upper poles, but, in reality, this does not work, despite the efforts of many plastic surgeons over the years to achieve it (Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128:1282–1301.). Breast tissue is simply too malleable. The failed notion of using breast tissue as a surrogate for a breast implant is called “autoaugmentation.” (Swanson E. Breast autoaugmentation: An enduring myth. Plast Reconstr Surg. 2015;135:779e–781e.) The good news is that implants perform very well in maintaining shape. The implant and the capsule that forms around it provide the firmness and durability that are needed to fill out the upper poles. In this situation, these “unnatural” qualities of the implant and capsule are working to our advantage. Indeed, it may be said (and I often do) that the bad thing about implants is that they are not just like breast tissue and the good thing about implants is they are not just like breast tissue.
The “Minus-Plus” Concept
Measurements show that mastopexies (the medical term for breast lifts) that just remove skin and do not remove breast tissue from the lower pole, the so-called “skin-only breast lifts,” are ineffective (Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128:1282–1301). Skin is simply too elastic to hold shape and the breasts typically remain “bottomed-out.” A better strategy is to remove extra breast tissue from the lower pole, where it is not needed, and add to the upper pole, where it is welcome. The only way to reliably increase upper pole fullness is by using implants. This is the “minus plus” concept originally described by Regnault and Daniel.
"I Like My Size and I Just Want a Lift”
Sometimes women say, “I’m satisfied with my size, I just want a lift.” Intuitively, one might think that these patients would be best served with a breast lift alone and no implants. But measurements show this is not the case (measurements again win out over intuition). These women need to know that if a breast lift is done properly, and extra breast tissue is removed from the lower pole along with skin, their breast size will actually decrease, and there will be no net gain in upper pole fullness. For this reason, I recommend implants for women who just want to maintain their size, usually of a modest volume. This is one reason it is much more common for me to perform augmentation/mastopexies than mastopexies alone. But there are other reasons too, and these are discussed later.

These illustrations, drawn to scale, depict the mean breast measurements before (left), after a breast lift alone (middle), and after a breast lift with implants (right). A breast lift alone corrects the sagging of the lower pole, but slightly reduces the breast size and does not fill out the upper pole. The breast does not appear to rise relative to the chest wall. An implant improves upper pole projection. The combination of an implant and a breast lift provides the appearance of a lifted breast.
In fact, mastopexies without implants are indicated only for women who want to correct sagging, and do not mind if their breasts are reduced a little in size, and accept wearing a bra to produce upper pole fullness. Or in women who simply don’t want implants.
So what if just skin is removed from the lower pole, preserving breast volume (a skin-only mastopexy)? The answer is not surprising. The patient may have the same breast size she had before, but it will still be saggy, so she is no better off. This fact explains the high rate of patient dissatisfaction after traditional breast lifts. It has nothing to do with unrealistic expectations, as is sometimes suggested. Flowers called this problem “the mastopexy-wrecking bulge,” referring to uncorrected lower pole excess in these patients. Experienced surgeons learn to remove not just skin, but breast tissue from the lower pole to avoid this problem.
Indeed, only an augmentation/mastopexy can provide the illusion of a breast lift. A mastopexy alone only tightens the lower pole and corrects the lower pole excess. For some women, this is enough. A mastopexy does not give the illusion of a breast that has been lifted up relative to the chest wall (see Illustration). Any woman who grabs her breasts from below and lifts up, saying “this is what I want,” should consider an augmentation/mastopexy.
Patients may have concerns about implants, which they may not have considered in the first place, but after being informed that they cannot expect to have unaided (no bra) youthful upper pole convexity without implants, and after looking at photographs of other women treated with and without implants, they often elect to have implants. In doing so, they are making an informed decision.
BREAST LIFT AND IMPLANTS (AUGMENTATION/MASTOPEXY)
The consistency of breast tissue changes with age—it loses its firmness. Women would like to restore the firm consistency they had as a teenager. Their breasts have lost firmness and the upper poles have flattened. Ideally, they would like to have a pleasing fullness of the upper part of the breasts, which they may have enjoyed when they were younger and before they had children. Of course, the consistency of the breast tissue is not changed by the lift. Patients wonder whether the lift itself can push their breast tissue up to round out the upper parts of their breasts. Unfortunately, a vertical breast lift alone provides minimal increase in upper pole fullness and an inverted-T approach (a method I used in the past but now consider obsolete) provides none. No matter how much the plastic surgeon pushes up on the tissues, the reality is that a breast lift alone does not fill out the upper part of the breasts.
If a patient desires greater firmness, or fullness in the upper poles and a fuller cleavage, implants are recommended. Most of my patients having a breast lift decide to have implants simultaneously. Implants may be inserted using the same incision used for the breast lift. Of course, this combined procedure introduces the possible complications of breast implants along with the benefits. The concept is “minus-plus,” more fullness where you need it (the upper poles) and less where you don’t (the lower poles).
Pregnancy
For those women who are planning to have more children, it is usually best to postpone a breast lift. The breasts will go through more stretching with another pregnancy and will lose tone. Although a breast lift may be retightened at a later date with no additional scars (the original vertical scar is removed along with extra skin), it is usually advisable to wait and have just one operation. However, this does not mean that a woman who is not sure if she will have another child in the future should put off this helpful procedure indefinitely, especially one that can make such a difference in self-esteem. Recommendations are individualized and, often in plastic surgery, there are exceptions to the rule.
Breastfeeding
A breast lift is unlikely to affect breast feeding capability. The ducts going from the breast tissue to their openings in the nipple are preserved. Only the extra skin is removed, and a small amount of breast tissue at the lower pole, so that breast function is usually maintained.
BREAST LIFT AND IMPLANTS (AUGMENTATION/MASTOPEXY)
Breast Lift and Augmentation
The consistency of breast tissue changes with age—it loses its firmness. Women would like to restore the firm consistency they had as a teenager. Their breasts have lost firmness and the upper poles have flattened. Ideally, they would like to have a pleasing fullness of the upper part of the breasts, which they may have enjoyed when they were younger and before they had children. Of course, the consistency of the breast tissue is not changed by the lift. Patients wonder whether the lift itself can push their breast tissue up to round out the upper parts of their breasts. Unfortunately, a vertical breast lift alone provides minimal increase in upper pole fullness and an inverted-T approach (a method I used in the past but now consider obsolete) provides none. No matter how much the plastic surgeon pushes up on the tissues, the reality is that a breast lift alone does not fill out the upper part of the breasts.
If a patient desires greater firmness, or fullness in the upper poles and a fuller cleavage, implants are recommended. Most of my patients having a breast lift decide to have implants simultaneously. Implants may be inserted using the same incision used for the breast lift. Of course, this combined procedure introduces the possible complications of breast implants along with the benefits. The concept is “minus-plus,” more fullness where you need it (the upper poles) and less where you don’t (the lower poles).
Breast Lift and Removal of Implants
Patients who have had breast implants in the past may wish to have them removed and have a lift done at the same time to tighten the breasts, which have been stretched by the presence of the implants. Without a lift, the breasts will look deflated after removal of the implants. A lift alone may be sufficient in women who had at least a moderate amount of breast tissue at the time of their breast augmentation, at least a B-cup size.
In patients who started with small breasts, it is best to replace the implants at the same time as the breast lift. Otherwise, the breasts will still look unfilled, even with a lift, and these women have gotten used to having something there to fill their bra. In this situation, which is a more common one, the breast implants will be replaced. The size of the new implants may be the same size, smaller, or larger than the original implants, depending on the patient’s wishes.
For women in their 40s and 50s, a large breast size may not be as desirable as it was when they were younger, particularly if the large breast size makes them look matronly. Their breast implants may be removed, replaced with smaller saline implants, and the breasts tightened as necessary with a breast lift. This gives the desired lean, but feminine, contour.
MOMMY MAKEOVERS
Breast Lift and Abdominoplasty
It is not unusual to combine a breast lift with other procedures, such as liposuction of the lower body or an abdominoplasty. Typically, women who have breast lifts have had children and their tummy has been stretched out along with their breasts. They may wish to have the tummy tightened at the same time their breast lift is performed. Both of these procedures are best performed after child-bearing to avoid restretching the tissues, so it often works out that the timing is right for both at the same time, a combination labeled a “mommy makeover.” The breast lift procedure is the less painful procedure. Women who have both procedures simultaneously are aware of their abdominal tightness and discomfort after the abdominoplasty, but barely notice any breast discomfort. Because the breast lift does not add much to the postoperative discomfort, and adds nothing to the recovery time, it makes sense to do it at the same time, avoiding a second operation.
Is Combining Surgery Unsafe?
Some plastic surgeons believe that combining procedures is unsafe. However, this view is not well demonstrated in the literature. Of course two procedures will have more complications than one, but the risk does not appear to be super-additive. It is important that any plastic surgeon doing combined surgery be proficient in the procedures done individually so that the surgery is not overly long and blood loss is not excessive.
Ideal Anesthesia
Safe anesthesia is a crucial element of elective plastic surgery. Plastic surgery is done under various forms of anesthesia. I prefer total intravenous anesthesia and use it for all of my procedures, even abdominoplasties and lower body lifts. The patient is asleep, but breathing spontaneously (not relying on a breathing machine), is not paralyzed, is not intubated (a tube is not inserted down between the vocal cords), and is not positioned prone (face down) during surgery. I call this “SAFE” anesthesia (Spontaneous breathing, Avoid gas, Face up, and Extremities mobile) (Swanson E. The case against chemoprophylaxis for venous thromboembolism prevention and the rationale for SAFE anesthesia. Plast Reconstr Surg Glob Open 2014;2:e160.) This type of anesthesia is also less likely to cause blood clots in the deep veins of the thighs. Patients tend to wake up quickly, are seldom nauseous, and are usually ready to go home 60–90 minutes after surgery. Sometimes patients worry that they might wake up during surgery. They can be reassured that, with this type of anesthesia, awakening during surgery is not going to happen, because the anesthetist would detect movement (the patient is never paralyzed) long before waking up. The patient wakes up in the recovery room, only minutes after surgery.
Breast Lift and Liposuction
For years, liposuction has been the most popular cosmetic surgical procedure now performed in the U.S., although breast augmentation may be even more popular today. Not surprisingly, many women combine breast surgery with liposuction of other parts of their bodies, usually the lower body, to balance their proportions. Liposuction helps with the transformation from a pear shape to an hourglass figure.
Click below for Photographs
"Before & After" Photographs of Breast Lift PatientsA Breast Lift Is Also a Breast Reduction and Vice Versa
The same technique is used in performing a breast lift and a breast reduction. In both cases, excess skin is removed to correct sagging. It is preferable when doing a breast lift to also remove extra breast tissue from the lower pole of the breast so as to adequately correct sagging. “Skin only” breast lifts do not hold up well over time because the skin is prone to stretching. So a breast lift is really a small breast reduction. Similarly, a breast reduction is also a breast lift because sagging is corrected. The only difference is how much breast tissue is removed. I (arbitrarily) use 300 grams per breast to differentiate a breast lift from a breast reduction.
The Importance of Technical Expertise
Technical expertise and proper procedure selection are of critical importance for surgeons performing breast lifts and reductions. In a breast augmentation, the surgeon’s skill largely comes to play in the proper dissection of the pocket for the breast implant. The incision is small and no alterations are being made to the nipple position. It is a procedure that many residents learn to perform competently during their training. It’s “Breast Surgery 101,” so to speak. Surgeons’ websites often contain dozens of pictures of breast augmentation. It is much less common to see dozens of pictures of breast lifts, and there is a reason for that.
Surgical expertise, results, and patient satisfaction are much more variable for breast lifts and reductions. To be proficient at a breast lift/reduction, there is no substitute for experience and correct procedure selection. This operation should not be done by a surgeon with no specialized training in plastic surgery. While there are areas of overlap in surgical specialties, this is not one of those areas. This operation is strictly in the domain of the plastic surgeon, preferably a plastic surgeon who specializes in cosmetic surgery and who performs this procedure regularly.
With advances in surgical technique and anesthesia, breast lift and reduction have become outpatient procedures, performed in an ambulatory surgery center or day surgery unit in a hospital. Experienced and skilled operators rarely find a need for a blood transfusion, overnight admission for healthy patients, or surgical times exceeding 3 hours.
Rule of 10
As you might expect, as the technical difficulty increases, the predictability and consistency of the result decreases (also true for rhinoplasty and facelift surgery). A review of the results of breast lifts and reductions on websites is informative. Patients know that the surgeon’s best results are on display. If these results appear unacceptable, the prospective patient should reconsider her options. A good rule of thumb is that you should see 10 examples of results you would be satisfied with. This way you can be assured that your surgeon has met your expectation level at least 10 times. Hopefully many more than that, but 10 is a good start.
How Much Breast Tissue Do You Take Out?
Patients often ask how I determine how much breast tissue to take out, or how much skin to remove. This is in the realm of the surgeon’s judgment. I make preoperative markings, but my final determination regarding tissue removal is made in surgery. To reduce the risk of persistent sagging, I have learned to take out more lower pole tissue and tighten more than I used to do. It is almost impossible to make the breasts too perky. Despite an overly-perky appearance right after surgery, the tissues always settle and the breast shape rounds out.
Nipple Grafts Are Obsolete
Some surgeons still use nipple grafts in some patients. This is an old technique that leaves the nipples completely numb and is unnecessary now that we have better options, particularly the vertical reduction with a medial pedicle (“pedicle” refers to the attachment of the nipple to surrounding tissue to maintain blood supply) which is safer than older techniques, like the inverted-T reduction, and less likely to jeopardize blood supply to the nipple.
The Incision
Because of its advantages in terms of less scarring, better shape, and shorter operating times, the vertical technique is preferred over the inverted-T (“anchor scar”) technique, both for breast lifts and reductions. The vertical technique is also safe to perform with breast augmentation, which is a common and highly gratifying combination procedure. Both the old inverted-T “inferior pedicle” procedure and periareolar procedures have design flaws. The inverted-T technique is prone to bottoming-out and flatness of the upper poles. The periareolar (“donut”) technique tends to cause distortion and flattening of the areola without a tightening effect for the lower pole. In order to avoid a persistent bulge of the lower pole of the breast, it is necessary to remove breast tissue and skin from the lower pole. If just skin is removed, the breast will remain bottomed-out. In fact, persistent sagging of the lower pole can sometimes occur even after a properly-performed vertical lift, and require a second operation to provide more tightening.
Preoperative Measurement and Marking
The surgeon first makes measurements on the patient’s chest. It is important that the patient sit up or stand squarely while the chest markings are made (not a good time for slouching), because the surgeon follows these lines closely at surgery. Except for the circular area around the nipple, all of the skin enclosed within these markings is removed. Patients are often surprised how much extra skin is present. The new nipple position will be located higher, at the level of maximum breast projection. This is determined in surgery. Markings help the surgeon create the tighter, more conical breast mound, and the nipple goes on top. This technique helps avoid locating the nipple too high on the breast, which is a common error and a difficult one to correct.
What Happens to the Nipple?
Patients often ask if the nipple is removed because pictures show an incision that goes circumferentially around the nipple, giving the illusion that it has been removed and then stuck back on at a higher position on the breast. In reality, it is the nipple that stays attached to the underlying breast tissue— the skin around it is removed. Patients with large areolae (the pigmented skin around the nipple) can have these reduced simultaneously. This is an extra benefit of the procedure and helps make the scar around the areola a more acceptable trade-off. The stitches dissolve on their own. There are no stitch marks or “railroad tracks”, because the “subcuticular” suture weaves back and forth under the skin.
The Surgery
Patients sometimes wonder if there will be an incision above the nipple. When I see women in consultation in the office, they sometimes grab the skin around the collarbone and pull it up tight, thinking that a breast lift will be done in a similar fashion (“Why can’t you just do this, doctor?”). In fact, this technique was tried in the early 20th century. But it is not used today, because the incision would be very conspicuous above the breast.
Why Not Stitch the Breasts Higher?
Patients sometimes wonder if stitches can be used on the inside to pull up the breast. This would be a nice way to accomplish the lift and avoid any scarring. Many surgeons have incorporated such sutures in their techniques. Unfortunately, these efforts have proved ineffective. Breast tissue is simply too malleable to be help up using deep stitches.
(Swanson E. A retrospective photometric study of 82 published reports of mastopexy and breast reduction. Plast Reconstr Surg. 2011;128:1282–1301.)
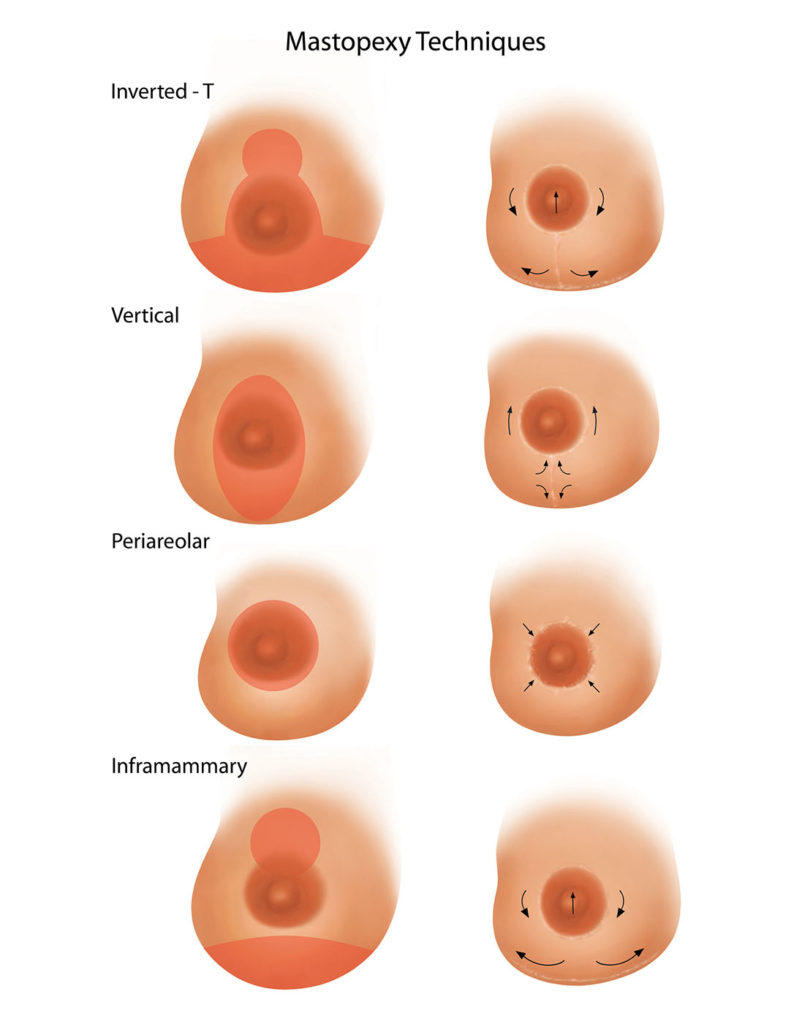
(photo information) Resection patterns for the inverted-T (top), vertical (second row), periareolar (third row), and inframammary (bottom) techniques. The breast dimensions are drawn to the actual mean values determined from a study of published results. The vertical technique has a sound rationale in geometry, removing tissue from the lower pole, and increasing projection by closing a vertical ellipse to a straight line. The inverted-T and inframammary techniques close a horizontal ellipse to a straight line, pulling the upper skin flap down in the process (necessitating nipple transposition) and widening the lower pole. The periareolar technique removes tissue from around the nipple/areola rather than from the lower pole where it is needed.
The Vertical Lift
To tighten the breast “envelope,” the surgeon removes skin and excess breast tissue of the lower pole, and this produces the lift. But unlike a facelift, where the skin is pulled up with the underlying SMAS tissue, in a breast lift the extra tissue is removed from below, and the sides are brought together, pushing the breast up. The vertical scar is kept below the level of the nipple so it does not show, even with low-cut tops or bathing suits.
The incision usually includes a circular part running circumferentially around the nipple and areola. This incision is needed so that the nipple and areola may be moved out of the way temporarily to perform the breast lift and then repositioned atop the newly shaped breast cone. With the vertical technique, the breast is elevated and the nipple comes up with it, so that transposition is minimal. This is important because the more the nipple is transposed, the more it is at risk of losing blood supply, which could cause a disastrous loss of the nipple. Older techniques, such as the traditional inverted-T with an inferior pedicle, often involved long pedicles. The vertical technique with a medial pedicle allows much shorter transposition distances (I call it nipple repositioning rather than transposition), with much greater safety for the nipple and areola. It also preserves superficial sensory branches to the nipple. These branches enter from the medial side (the side facing the other breast).
The Periareolar (Donut) Approach Is Usually Insufficient
The nipple and areola are freed of the surrounding skin. In one operation, called the periareolar or “donut” mastopexy, the skin is removed as a ring around the areola. Although this approach is appealing in its simplicity and avoidance of a scar below the nipple, it is limited in how much sagging it can correct. Most patients require tightening of the lower pole, so this incision is rarely used. My only indication is an occasional patient who wants her areolar size reduced but does not require a lift.
“Crescent mastopexies” tend to distort the areola without any tightening of the lower pole or improvement in breast shape. The extra skin is removed from around the areola, rather than from the lower pole, where reduction is needed to improve shape. Such “periareolar techniques” that avoid a vertical scar are therefore of limited usefulness. I will use it sometimes to move a nipple slightly in cases of minor asymmetry.
If a patient requires any degree of lift, and almost all do, then the vertical procedure is the better choice.
The Inverted-T (Anchor Scar) Approach Is Obsolete
Many North American plastic surgeons, including myself, were trained to perform breast lifts and reductions using the old inverted-T method, which leaves a scar in the shape of an anchor. This method has a number of design flaws. My measurement studies showed that breasts tend to look flattened, square, and the nipples are overelevated. Ironically, breasts after this type of lift or reduction tend to resemble preoperative breasts for vertical augmentation/mastopexy. Fortunately, using a combination of a vertical lift and implants, this unfavorable breast appearance can be remedied.
Also, the horizontal scar is long and prone to widening on the sides where it might be seen. The blood supply to the nipple is jeopardized, increasing the risk of catastrophic nipple loss. Inserting a breast implant can further restrict blood supply by adding pressure, increasing the risk of tissue loss (For this reason, there are surgeons who believe the combined lift/implant procedure is unsafe. The problem is not combining procedures. The problem is an invalid breast lift operation with a narrow margin of safety that is tested by adding a breast implant.) There is also a higher rate of nipple numbness because many of the sensory nerves supplying the nipple are sacrificed. For all these reasons, there is a growing number of surgeons, like myself, who believe that it is time to leave this operation for the history books.
The vertical technique makes use of a vertical extension from the areola to the crease under the breast (“inframammary crease”), allowing tightening from side-to-side. This leaves a scar around the areola, plus a vertical scar down to the crease. The inframammary crease is usually elevated. I may use a short inverted-T modification at the bottom of the vertical scar if it appears that the scar might otherwise extend too far down onto the abdomen where it might be visible. This scar is much shorter than the horizontal component of the “anchor scar.”
Redo Breast Lift
Occasionally, a breast lift may be redone. This may be necessary because of gradual stretching of the breast skin over time, or if implants are removed in a woman who has had a previous breast lift. It may also be done when there is a persistent bulge of the lower pole. The original vertical scars are removed along with the extra skin. It may not be necessary to make another incision around the areola if the nipple is at the correct level. If the patient had a previous inverted-T lift or reduction, this horizontal scar may be shortened. Most women treated with a previous inverted-T mastopexy or reduction are candidates for reoperation using the vertical technique to tighten the lower poles, correct boxiness, reduce the extent of the horizontal (“anchor”) scar, and restore upper pole volume using implants.

*Swanson E. Prospective outcome study of 106 cases of vertical mastopexy, augmentation/mastopexy, and breast reduction. J Plast Reconstr Aesthet Surg. 2013;66:937–949.
Christina’s Surgery
Before Surgery
Christina, age 26, developed breast sagging after having two children. She was referred by her mother-in-law, a former patient. Christina wished to have a similar breast volume, just repositioned, like she was before her pregnancies. She decided to have a breast lift with implants to correct the sagging and restore fullness to the upper poles of her breasts.
Two weeks before surgery, she attended her preoperative appointment. Her blood test was performed. She received prescriptions for painkillers and antibiotics. She was given preoperative instructions. She knew not to eat or drink anything the morning of surgery.
Day of Surgery
Christina and her husband arrive at the surgery center 1 hour before her scheduled surgery time. She is met by the circulating nurse, also a former patient, and changes into a gown. The nurse checks her vital signs. Dr. Swanson takes photographs and marks the breasts.
Next, the anesthetist meets with Christina and starts the I.V.

Christina walks to the operating room, her I.V. already started. The operating nurse has already prepared the table with sterile instruments.

In the operating room, Christina lies down on the operating table. The anesthetist puts on a blood pressure cuff and applies the EKG leads and an oxygen monitor.

At the head of the table, the anesthetist opens a vial of a milky substance (propofol) and loads it into an infusion pump. The medication makes its way through the I.V. tubing. The anesthetist tells her to pick out a nice dream and Christina falls asleep. The anesthetist inserts an airway and administers oxygen.

Christina is now asleep, but breathing on her own. Dr. Swanson injects local anesthetic and proceeds with the surgery.

Two hours later the surgery is over. The nurses apply the dressings and Christina is transferred to the recovery room. The recovery room nurse will be looking after her as she wakes up.
Within 10 minutes, Christina is wide awake. Dr. Swanson checks in on her. She’s smiling. She feels better than she had anticipated and is not having pain. The local anesthetic used in surgery and the I.V. medications are working well. The nurse checks her breasts—no unusual swelling.
photo with Dr Swanson in recovery room

Her husband joins her in the recovery room. The nurse checks her vital signs one more time and helps her to the bathroom. She gets dressed and ready to go. The nurse gives her husband the postoperative instructions. A short wheelchair ride and she gets in her car. She’ll be back tomorrow for her follow-up office visit.

Recovery
Patients are often pleasantly surprised that there is not as much discomfort as they expected after a breast lift. Usually, there is not a great deal of pain with this procedure. In fact, the average pain rating is a moderate 4.2/10, likely because there is no deep dissection into the breast tissue and the muscle is not lifted. Patients take painkillers for 6 days, on average, are back to work in 6 days, and report feeling “back to normal” in 1 month.
However, if a breast augmentation is performed simultaneously, there is more discomfort from stretching the muscle to place the implants. The average pain rating reported by a patient after a breast lift with implants is 5.3/10. A breast lift and augmentation is typically no more painful than a breast augmentation alone. The average pain level after a breast augmentation is 5.9/10. The recovery experience is virtually identical.
I do not use drains in performing breast surgery. The dressings come off when the patient returns to the office on the day after surgery. Patients may then start bathing right away. The incisions are covered by small semi-transparent adhesive strips (“Steri-Strips”) which stay on even during bathing. A light gauze dressing is inserted in the bra for comfort and to collect small amounts of fluid which ooze from the wound. This tissue fluid usually stains the gauze yellow and is normal. The Steri-Strips come off at the second office visit, usually 1 week later. Sometimes they start to peel off sooner, and that is okay. They are an extra precaution and are not even used in patients who are allergic to them. The soft sports bra is worn day and night for a month, and then according to patient comfort, on during the day and off at night. Underwire bras are avoided for at least a month to avoid any undue pressure on the incisions while they are healing. A moisturizer may be used to treat dry skin. A topical antibiotic such as Neosporin is used to treat any areas of crusting or delayed healing after the Steri-Strips come off.
Swelling
The breasts swell right after surgery. They may feel tight and look unnatural—flat across the bottom rather than rounded, with excessive upper fullness and an indistinct cleavage. This is due to swelling and skin tightness. These findings are expected. Gradually the swelling dissipates and the tissue relaxes. Over the next few months, the breasts will settle and look more pendulous and natural. Bruising can take several weeks to clear.
Numbness
Because the skin is cut during the procedure, small sensory nerve branches in the skin are divided. Gradually these tiny nerve endings regenerate and the feeling gradually returns. Nipple sensation usually remains intact, because the nerves that supply it from below are preserved. (In a breast lift, it is the surrounding skin which is removed while the nipple itself is left attached to the underlying breast tissue). However there may be loss of feeling in the nipples, usually temporary, particularly if breast implants have been used, because there has been more stretching of tissues and nerves.
Activity
Although the usual time period off work is 1 week, many women resume working after 3 or 4 days, provided they have a sedentary job. Jobs requiring physical activity (waitress, factory worker, etc.) will have longer recovery times, up to 3 weeks. Women can walk right away, and walk a few miles, to maintain fitness about 2 weeks after surgery. Exercise involving upper body activities should be avoided for 1 month, when patients may resume full physical activity.
Today, interruption of exercise is an important issue for many women, which is a good sign in a society that is plagued by a high rate of obesity. After implant surgery, women notice how much they use their pectoral muscles in everyday life, whether it’s lifting bags or pushing open doors. Even the use of light weights for doing biceps curls involves the pectoral muscles. There is no advantage in overdoing exercise early after surgery. Exercising too soon causes unnecessary increased swelling and discomfort (usually felt after the workout, not during), and may prolong the healing time.
Scarring
Like all scars, particularly on the body (as opposed to the face where scars generally heal well), breast scars may widen. There is certainly a genetic component to this, and clues may be obtained from other scars on the body, especially the abdomen. How did the appendectomy or Caesarean section scar turn out? If a patient has a nicely healed and inconspicuous abdominal scar, chances are their breast scars will do well too. However, if they heal with thick, raised hypertrophic scars or are prone to keloids, their breast scars are likely to be similarly affected. In this situation, it may be best not to have the surgery—the balance is too much on the cost side (unsightly scars) and not enough on the reward side (improved breast shape).
Surgery creates some tension on the scars. Tension tends to make them widen. Later, when the tension has reduced by relaxation of the tissues, the scars may be revised if necessary under local anesthesia. If a scar revision is recommended, it is usually performed at least several months after the breast lift.
Scarring and the Inverted-T Method
The horizontal scars left by the older inverted-T technique can often be seen running close to the middle of the chest and on the sides where they may not always be concealed by the inframammary crease. Patients find these scars the most objectionable of the three scars (periareolar, vertical, and horizontal) that are part of the old inverted-T anchor incision.
Improved Scar Using the Vertical Technique
The vertical technique is often called a “short scar” method by plastic surgeons. This name suggests that the difference between this technique and others is simply a more limited scar, although, as we have discussed, the advantages go beyond less scarring and include improved shape. The vertical scar often heals nicely, although it is not unusual to have small areas of delayed healing.
Puckering or “Dog Ears”
There is a pucker (“dog ear”) at the bottom of the vertical scar. This is created when an ellipse of tissue is removed above it. The only way to avoid such puckering is by making the incision longer. Of course, we don’t want to make the incision any longer because we want to limit the length of the incision so as not to leave a scar continuing down on to the abdomen. However, it is sometimes necessary to come back and treat a persistent dog ear by cutting out a small area of puckering that does not completely flatten out. I do not hesitate to use a short horizontal modification at the bottom of the vertical scar to keep the scar from extending onto the abdomen. Even with diligent surgery and follow-up care, scars may widen. But they will look better with time. They will soften and the redness will gradually fade.
Persistent Lower Pole Fullness
This is the most common complication of a breast lift. It is usually caused by inadequate removal of breast tissue from the lower pole of the breast, so that there is a persistent bulge of the lower pole, which one surgeon colorfully calls the “mastopexy-wrecking bulge.” This problem is common among patients treated with “skin-only mastopexies” because the skin stretches readily and cannot hold the breast shape. It is also commonly found in patients treated with “periareolar” or “donut mastopexies” because these techniques do not allow removal of breast tissue from the lower pole. They do avoid a vertical scar, leaving just the scar around the areola, which is the appeal of these limited-incision techniques, but this benefit is outweighed by the inability of these techniques to adequately tighten the lower pole and provide a lift.
Infection
As in any surgery, infection is a risk. Patients receive intravenous antibiotics at the beginning of the operation. After surgery, they take antibiotics for 24 hours. This is short course of antibiotics recommended to help prevent infection. Longer periods of “prophylactic” antibiotics used in the past may be counterproductive, providing more opportunity for emergence of resistant organisms.
T.C., Age 45, Wellness Coach
Height: 5’6″
Weight: 166
Children: 2
Right Breast Tissue Removed: 434 g
Left Breast Tissue Removed: 165 g
Placement: Submuscular
Implant Size: Right: 420 cc/Left: 570 cc
Implant Type: Mentor smooth, round, moderate-plus profile, saline
Comments: This 46-year-old patient developed a superficial infection (cellulitis) of her left breast after a breast lift with implants. The signs of infection were present—increased redness, tenderness, and a mild fever (99.1° F). The infection cleared with oral antibiotics. She did not need to have her implant removed. She was left with a small area of increased scarring along her left areola that did not require revision. Her breast asymmetry was corrected. For the first time in 30 years, she no longer needed to wear an insert in her left bra cup. Despite her complication, she came to a successful outcome. Fortunately, this is true of most complications that are properly managed.

Before, 3 weeks after, 3 months after
Hematoma
Because the dissection is superficial, hematomas are uncommon for breast lifts alone (but may be due to the breast augmentation if this is done at the same time) and are signaled by marked discomfort and swelling, usually on one side, within the first 24 hours after surgery. Recognition is the key. If a hematoma is diagnosed, the patient returns promptly to the operating room for evacuation of the hematoma, which provides immediate relief. An excellent outcome can still be achieved with prompt treatment of this complication.
Skin Loss/ Delayed Healing
Because skin circulation is partially interrupted by raising skin flaps, avoidance of smoking is important to reduce the risk of loss of skin along the wound margins. (This is true in any procedure which involves raising skin flaps, such as facelift, abdominoplasty, and at least with past techniques, breast lift/reduction). The risk of skin loss is reduced if skin undermining is avoided and pedicle dissection is minimized, which is the case for the vertical technique but not the inverted-T. For this reason, smoking is not a contraindication for a vertical lift or reduction. However, it is best to keep the odds in our favor, so smokers are still instructed to stop smoking 2 weeks before and 2 weeks after surgery. Smoking cessation patches and gum also contain nicotine, the substance which causes the small blood vessels to tighten, so these also need to be avoided.
If a small margin of skin loss occurs, the patient is reassured and instructed to keep the open area clean with soap and water, apply antibiotic ointment and a light gauze dressing. The wound is allowed to heal in on its own. Because wounds contract in from the sides and shrink as they heal, the resulting scar is often surprisingly small, and usually requires no treatment. Scars that widen as they heal may be treated later with a scar revision.
Although rare, it is possible to also lose portions, or all of the areola and nipple. Anything that interferes with circulation to the skin such as excessive tightness, an underlying hematoma, pressure on the skin, or smoking (due to nicotine), can lead to this complication, which is best avoided.
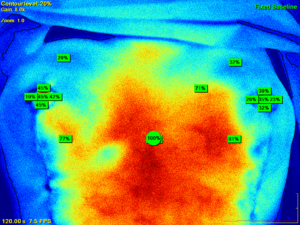
Augmentation/Mastopexy—Does It Pose Extra Risk?
Some surgeons have expressed concern about combining a breast lift and implants, citing high complication rates, higher than what might be expected if the operations were done in stages. However, our study and others show no higher rate of complication rates for the combined procedure. I studied blood supply to the breast skin, including the nipples and areolae, and found that adding implants did not significantly diminish blood supply if the vertical technique is used. (Swanson E. Safety of vertical augmentation/mastopexy: Prospective evaluation of breast perfusion using laser fluorescence imaging. Aesthet Surg J. 2015;35:938–949.)
Problems may be encountered when a surgeon uses a periareolar or inverted-T technique with implants because of the technical deficiencies of these techniques, which lead to a higher complication rate. Vertical mastopexy in combination with implants is safe and the combination procedure has a number of advantages over either operation alone. Any woman who is a candidate for a breast lift or augmentation done individually is a candidate for the combined procedure.
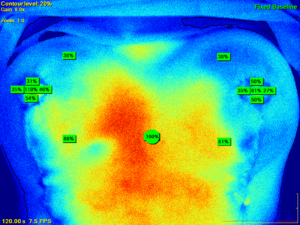
These laser fluorescence images show blood supply to the breasts, and specifically the nipples, during surgery. The image on top was taken after the mastopexy was performed but before implant filling. The image on the bottom was taken after the implant was filled. There is no reduction in blood supply, indicating safety of combining implant placement at the time of a mastopexy, as long as the vertical method is used in performing the mastopexy.
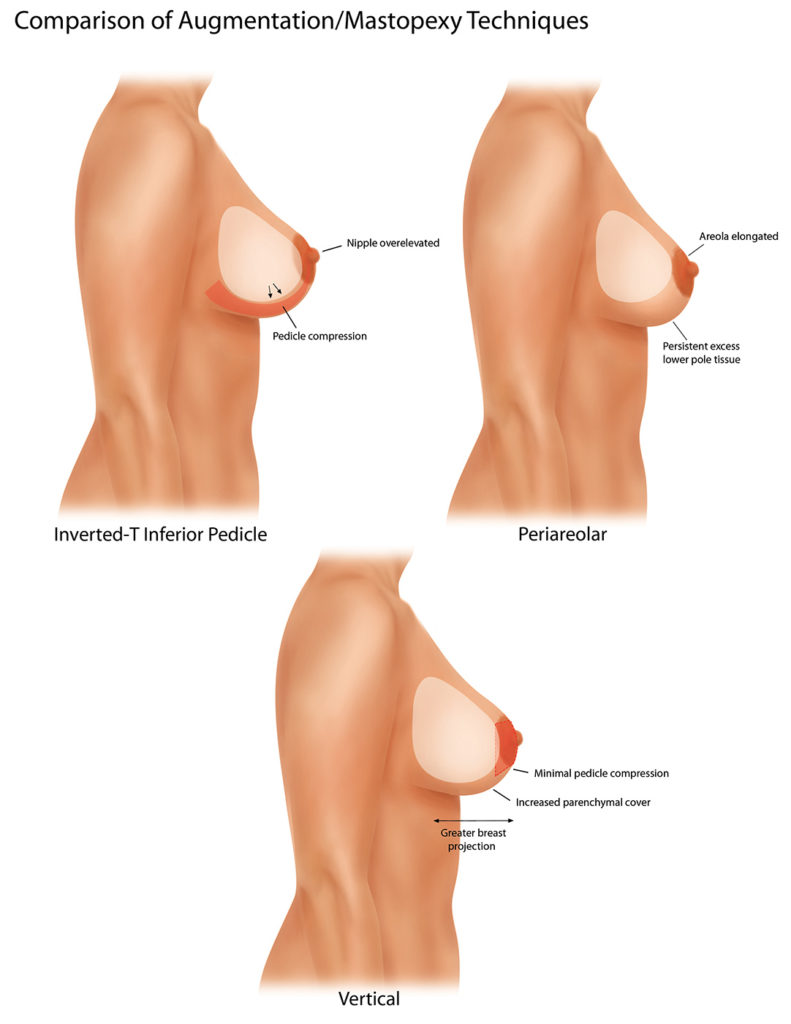
This illustration compares augmentation/vertical mastopexy to augmentation in combination with inverted-T and periareolar resections. The inferior pedicle of an inverted-T procedure is prone to pedicle compression and nipple overelevation. The periareolar procedure does not address lower pole excess tissue and places excessive tension on the periareolar scar. The vertical procedure treats lower pole excess, avoids pressure on the pedicle, and provides tissue cover over the implant.
- (Swanson E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast Reconstr Surg. 2013;132:30e–45e; discussion 46e–47e.)
At the time of your follow-up appointment at the office, the dressings are removed. The semitransparent tapes on the skin (Steri-Strips) are left on and your bra is put back on with gauze inserts. You can replace the gauze pads as necessary. It is now okay to start bathing. If any of the Steri-Strips come off in the water, that’s okay. Wear the bra both day and night for 2 weeks for comfort and protection. Lie on your back to sleep. Avoid lying on your tummy or side for a few weeks until this becomes comfortable. Allow at least 1 month before sleeping on your tummy.
The stitches dissolve on their own. Sometimes suture ends that become exposed are trimmed by your surgeon or assistant at the time of your follow-up visit. Antibiotic ointment such as Polysporin or Neosporin may be applied to any open areas or crusts, twice a day.
Q: I don’t really want implants. I’m not in favor of artificial materials in my body and I’m concerned about the safety.
A: You may consider saline-filled implants. If they leak, it’s just water, which is not harmful (although some women report symptoms of Breast Implant Illness after having saline implants). Or just have a breast lift and forego implants.
Q.How do you know what size to use?
A. Many women show me photos on their mobile device, which is helpful too.
Q: What incision do you use?
A: Inframammary: The incision is located on the lower part of the breast, just above the crease under the breast. My second choice is periareolar, making use of the natural border around the areola to hide the scar. I rarely use the axillary incision that leaves a scar in the armpit. It is more difficult to dissect the breast pocket because the incision is more removed from the area of dissection.
Q: Over the muscle or under the muscle?
A: Under the muscle. The breast appears more natural, feels more natural, and there is less risk of a capsular contracture.
Q: Do you use contoured implants?
A: No. As it turns out, it’s hard to tell any difference between round and contoured implants when they are in the body. Contoured implants are textured and I prefer smooth implants because they don’t leak as much and are less likely to cause seromas (fluid collections) later on. Contoured (shaped) implants cause disproportionately greater fullness of the lower poles, and may rotate, causing asymmetry. Also, contoured implants are more expensive.
Q: Do I have to have my implants changed out every 10 years?
A: This is a common question. No, there is no need to have breast implants replaced in 10 years. If you do not have a deflation, they may last much longer than 10 years. Nevertheless, you should count on having another breast operation at a future date, whether it is in 6 months or 15 years, we do not know. The most common reasons are to change to a different size (usually larger), release a capsular contracture, or to replace a deflated implant.
Q: Will I lose feeling in my nipples?
A: Forty percent of patients report at least temporary decreased sensation of their nipples, but it almost always returns to normal.
Q: Should I wait until after having children ?
A: There is no medical reason to wait.
Q: Can I still breastfeed?
A: Breast augmentation does not interfere with your ability to breast feed. Keep in mind that not all women can successfully breast feed. However, if you’ve successfully breastfed your children before, it is likely that you will still be able to nurse after your augmentation.
Q: Should I have a mammogram first?
A: Recommendations regarding mammograms do change from time to time. If you are due for a mammogram, have it done before your breast augmentation. You can have mammograms after the breast augmentation, but it is best to schedule this at least 6 months after your breast augmentation, unless there is a medical reason (like a lump) to do so earlier.
Q: What is the risk of deflation?
A: About 1–3% over 10 years for saline-filled implants.
Q: Silicone or saline?
A: Both work well. The appearance is very similar and any feel advantage for silicone gel is made less by the overlying tissue. However, if you are very thin and have very little breast tissue, and are concerned about wrinkling, you may consider silicone gel.
Q: How do you know what size to use?
A: The selection of size is more art than science. Although there are measurement systems available, these tend to underestimate implant size. Inserting implants in the bra is not particularly helpful because this does not accurately reflect the change in size that is created by an implant that is placed in the body.
Ideally, the patient achieves the size she wants in one operation. After talking with my patient, examining her, and looking at pictures of other patients with her, I have a good idea what she wants. Some women bring magazine photos or show me photos on their phone, which is helpful too.
In my practice, almost no one says they are too large at the time of their 1-month follow-up appointment. I do have the occasional patient that wants to be larger. Over a 5-year period, five patients returned for larger sizes. No one returned to have the implants changed to a smaller size. It is often difficult even for patients to know what size they want before surgery. Some patients become more appreciative of their breasts after surgery and less inhibited about a larger size.
Q: When can I return to work?
A: Most patients return to work in a week, but there certainly is a range. Some women get back to work in a few days and others are glad they took a week off. If you have a physical job, 2 to 3 weeks off is better.
Q: Do you use a pain pump?
A: No. Although it sounds like a good idea, “pain pumps” (actually local anesthetic infusion devices) have not worked well in practice. Patients find them cumbersome and pain scores with the pump were not significantly better than patients treated without a pump in a controlled double-blind study.